In recent years, the intersection of psychological stress and reproductive health has drawn significant attention from researchers, particularly concerning its implications for women suffering from polycystic ovary syndrome (PCOS). A groundbreaking study conducted by Mo et al. investigates how chronic psychological stress can disrupt reproductive and metabolic functions, specifically through the role of a regulatory protein known as kisspeptin. This research not only enhances our understanding of PCOS but also highlights the urgency for effective management of psychological stress in women diagnosed with this condition.
The findings underscore the complex relationship between emotional well-being and physiological health. PCOS is a multifaceted endocrine disorder that affects approximately 6-12% of women of reproductive age. Characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries, the syndrome has been linked to various metabolic disturbances, including insulin resistance and obesity. However, recent evidence points to psychological stress as a significant exacerbating factor. What Mo et al. bring to light is the exact biochemical pathway connecting chronic stress to the dysregulation of reproductive and metabolic functions in this population.
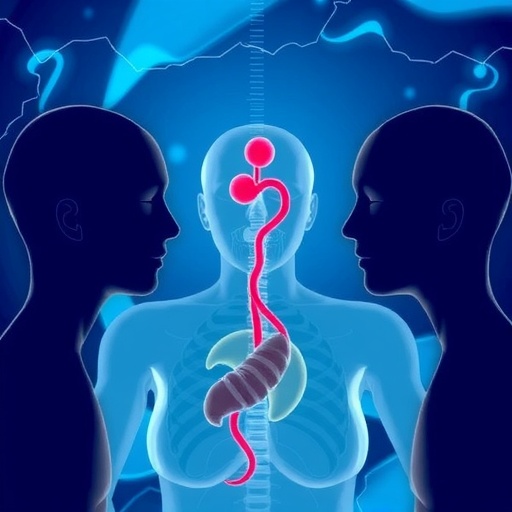
Kisspeptin, a neuropeptide encoded by the KISS1 gene, has emerged as a crucial player in the regulation of the reproductive hormone axis. This protein is primarily known for its role in triggering the release of gonadotropin-releasing hormone (GnRH), which in turn stimulates the secretion of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These hormones are pivotal for normal reproductive function, and any disruption can lead to the symptoms observed in PCOS.
In this study, the researchers employed both human and rat models to explore how chronic stress affects kisspeptin levels and, consequently, reproductive health. The evidence gathered suggests that psychological stress elevates levels of kisspeptin, which then impacts the hormonal balance necessary for regular ovulation. This finding not only establishes a direct link between stress and reproductive health but also opens avenues for novel therapeutic strategies targeting kisspeptin as a potential intervention.
Moreover, the metabolic implications of increased kisspeptin signaling cannot be overlooked. The study draws parallels between reproductive dysregulation and the heightened risk of metabolic disturbances often seen in women with PCOS. These include symptoms such as dyslipidemia and an increased propensity for developing type 2 diabetes. The findings indicate that chronic stress-induced changes in kisspeptin levels could set off a cascade of negative metabolic effects, compounding the health challenges faced by women with this condition.
The research also delves into the physiological mechanisms at play. Chronic stress is known to alter the hypothalamic-pituitary-gonadal (HPG) axis, which is essential for reproductive health. The dysregulation of this axis results not only in altered hormone levels but can also lead to conditions such as chronic inflammation, which further exacerbates PCOS symptoms. By understanding the role of kisspeptin in this context, we gain insights into how lifestyle interventions aimed at reducing stress could mitigate some of the reproductive and metabolic dysfunctions associated with PCOS.
Additionally, the implications of this study extend beyond mere hormonal balance. The role of kisspeptin as a mediator suggests potential for more multidisciplinary approaches to treatment. For instance, integrating psychological support and stress management strategies within the clinical framework for PCOS could potentially lead to improved health outcomes for women suffering from this syndrome. This aligns with emerging trends in medical research that advocate for holistic treatment paradigms.
The findings presented by Mo et al. are timely, as they coincide with a growing recognition of the importance of mental health in chronic health conditions. As PCOS affects a significant number of women, the need for more nuanced approaches to their care is paramount. The research advocates for healthcare providers to not only focus on the physical symptoms, such as irregular menstrual cycles and metabolic dysregulation, but also consider the psychological factors that may be at play.
Furthermore, the need for public health initiatives that raise awareness about the significance of managing stress in women with PCOS cannot be overstated. By educating patients and healthcare providers about the consequences of chronic psychological stress, a proactive approach can be adopted that may ultimately improve both reproductive and metabolic health.
Given the complexity of PCOS, future research should aim to further elucidate the mechanisms by which kisspeptin impacts both reproductive and metabolic health under stress. Longitudinal studies involving diverse cohorts of patients will be essential to ascertain the generalizability of these results. Such investigations could lead to the establishment of clear clinical guidelines for the integration of psychological support in the treatment of PCOS.
As we venture into an era where the interconnection between mental and physical health is more recognized, studies like this one by Mo et al. serve as crucial stepping stones toward advancing our understanding and improving care strategies for complex syndromes such as PCOS.
In conclusion, the study by Mo et al. offers a fresh perspective on the intricate web linking psychological stress, kisspeptin, and reproductive/metabolic health in women with PCOS. By advancing our knowledge in this area, we open doors to potential interventions that align mental and physical health strategies, paving the way for improved quality of life for affected individuals.
In light of these emerging insights, it is imperative that researchers, clinicians, and policymakers work collaboratively to address the multifactorial challenges faced by women with PCOS, ensuring that both psychological and physiological needs are met comprehensively.
Subject of Research: The impact of chronic psychological stress on reproductive and metabolic dysregulation in polycystic ovary syndrome, mediated by kisspeptin.
Article Title: Kisspeptin mediates the impact of chronic psychological stress on reproductive and metabolic dysregulation in polycystic ovary syndrome: evidence from human and rat models.
Article References:
Mo, T., Qiu, Y., He, S. et al. Kisspeptin mediates the impact of chronic psychological stress on reproductive and metabolic dysregulation in polycystic ovary syndrome: evidence from human and rat models. J Ovarian Res (2025). https://doi.org/10.1186/s13048-025-01918-6
Image Credits: AI Generated
DOI: 10.1186/s13048-025-01918-6
Keywords: Polycystic ovary syndrome, kisspeptin, psychological stress, reproductive health, metabolic dysregulation.