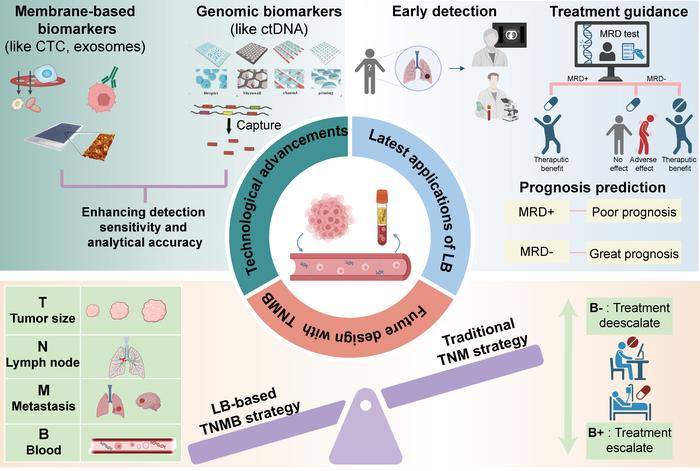
This study was led by Kezhong Chen (Department of Thoracic Surgery, Peking University People’s Hospital & Peking University People’s Hospital Thoracic Oncology Institute). In clinical practice, traditional tumor-node-metastasis (TNM) staging had difficulty achieving accuracy in prognosis stratification at the individual patient level. Researchers therefore proposed to introduce blood minimal residual disease (MRD) status and proposed a new tumor-node-metastasis-blood (TNMB) staging system to more accurately and individually define the postoperative status of lung cancer patients (Fig. 1).

Credit: ©Science China Press
This study was led by Kezhong Chen (Department of Thoracic Surgery, Peking University People’s Hospital & Peking University People’s Hospital Thoracic Oncology Institute). In clinical practice, traditional tumor-node-metastasis (TNM) staging had difficulty achieving accuracy in prognosis stratification at the individual patient level. Researchers therefore proposed to introduce blood minimal residual disease (MRD) status and proposed a new tumor-node-metastasis-blood (TNMB) staging system to more accurately and individually define the postoperative status of lung cancer patients (Fig. 1).
LB, well known for its noninvasiveness, easy accessibility, reproducibility, and ability to comprehensively and dynamically display tumor data, exhibits promising potential in the early detection, treatment evaluation, prognosis, and recurrence monitoring of non-small cell lung cancer (NSCLC). In recent years, with the rapid progress and developments in these technologies, LB has demonstrated promise as a new approach to break through the clinical bottlenecks described above.
The low dropout rate of LB biomarkers, the existence of background noise such as clonal hematopoiesis, and the lack of unified standards are still problems. Herein, researchers present a comprehensive overview of the technical updates implemented to address the aforementioned issues and propose an innovative and practicable approach for the precise management of NSCLC following LB integration.
Biomarkers like circulating tumor cells (CTCs) and exosomes which possess unique characteristics while sharing a common lipid bilayer structure and containing abundant genetic and proteomic information protected by this bilayer, overlap in the techniques for enriching and distinguishing these vesicles. Detection methods for genetic information based on cell-free DNA (cfDNA) can be categorized into PCR-based and next generation sequencing (NGS)-based approaches. Researchers summarized the methods used in the current study to increase the detection rate of genetic information and improve the accuracy (Fig. 2).
Researchers proposed the development of a TNMB staging system that incorporates information from the blood to enhance the current TNM cancer staging system. This novel component will promote further advancements in precision oncology. In the past, due to methodological limitations, numerous false negatives emerged, and existing clinical trials were solely designed based on TNM staging or MRD detection. However, the utilization of personalized panels and the development of sequencing techniques, exemplified by the PROPHET study, has significantly enhanced detection sensitivity and validated the advanced nature and efficacy of integrating liquid biopsy information into the tumor TNMB staging scheme. Consequently, if the technology can be standardized, it is conceivable that future clinical trials could be constructed based on TNMB staging (Fig. 3). Anticipated that with advancements in mechanism development and detection technology, LB technology will gradually gain acceptance in the management of NSCLC.
###
See the article:
Development of new techniques and clinical applications of liquid biopsy in lung cancer management
Journal
Science Bulletin