In a groundbreaking study that promises to reshape our understanding of neurodegenerative diseases, researchers have unveiled a critical role for microglia-derived β-hexosaminidase in maintaining neuronal health, particularly within the context of Sandhoff disease. This devastating lysosomal storage disorder, characterized by the toxic accumulation of GM2 gangliosides due to enzyme deficiency, has long posed significant challenges for clinicians and scientists alike. Now, through innovative approaches involving microglial replacement in a genetically engineered mouse model, the scientific team led by Tsourmas et al. offers revolutionary insight into how the brain’s innate immune cells contribute not only to pathology but also to neuronal survival and function.
Sandhoff disease belongs to a family of lysosomal storage disorders distinguished by mutations affecting β-hexosaminidase A and B, enzymes responsible for the breakdown of gangliosides within lysosomes. Deficiency in these enzymes leads to an unparalleled build-up of GM2 gangliosides, causing progressive neurodegeneration, motor dysfunction, and ultimately premature death. Historically, efforts to combat Sandhoff disease have tried to target the neurons themselves or to enhance systemic enzyme replacement, yet the blood-brain barrier and the complexity of neural tissue have imposed daunting obstacles. The latest findings suggest that microglia, specialized myeloid cells resident in the brain, may hold an unexpected key to enzyme delivery and neuronal rescue.
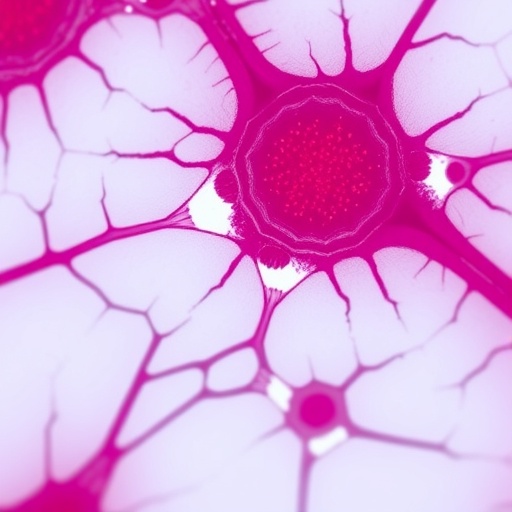
Microglia, the brain’s resident immune cells, are critical regulators of neural homeostasis and responses to injury. Traditionally viewed primarily as mediators of inflammation, recent research has gradually expanded their recognized functions into realms of synaptic pruning, neuroprotection, and trophic support. However, the role of microglia as reservoirs or vectors of enzymatic activity toward neurons remained largely speculative until now. Tsourmas and colleagues pursued an elegant strategy to directly test the impact of microglia-derived β-hexosaminidase on neuronal function by employing microglial replacement therapy in a mouse model deficient for this crucial enzyme.
The methodology was highly sophisticated: utilizing genetic ablation of native microglia followed by transplantation with donor microglia competent for β-hexosaminidase expression, the researchers were able to dissect the contributions of these immune cells from neuronal and global systemic sources. Comprehensive analysis spanning behavioral assays, biochemical quantification, and histopathological assessment revealed that microglial replacement effectively restored β-hexosaminidase activity within the brain milieu. Remarkably, this enzymatic restoration correlated with decreased GM2 accumulation, improved neuronal viability, and ameliorated motor deficits—hallmarks that have previously remained intractable.
This result fundamentally challenges the notion that enzyme activity limited to neurons or astrocytes governs Sandhoff pathology. Instead, a paradigm emerges wherein myeloid-derived β-hexosaminidase, secreted or transferred locally by microglia, constitutes a vital support system for neuronal health. Precisely how this enzyme transfer occurs poses fascinating mechanistic questions. The study provides evidence suggestive of microglial exosome-mediated delivery or direct uptake through enzymatic cross-correction pathways, allowing neurons to supplement their own otherwise deficient enzyme pools.
Importantly, the study’s comprehensive approach included temporal analysis demonstrating that earlier intervention with microglial replacement yielded more pronounced benefits. This finding underscores the progressive, window-dependent nature of enzyme deficiency pathogenesis and suggests that timely correction within the brain’s cellular ecosystem is paramount. Moreover, transcriptomic profiling of replacement microglia indicated enhancements in anti-inflammatory and neurotrophic pathways, which may synergize with enzymatic support to augment neuronal repair mechanisms and delay disease progression.
These results carry profound translational implications, positioning microglial replacement as a promising therapeutic avenue not only for Sandhoff disease but potentially for a spectrum of lysosomal storage disorders and other neurodegenerative diseases characterized by enzyme deficiencies or impaired intercellular trafficking. The concept of harnessing or engineering myeloid cells to deliver critical enzymes or molecular cargo inside the brain opens new frontiers for cell-based therapies—a significant leap beyond traditional gene therapy or systemic enzyme replacement strategies.
Yet, the journey from these preclinical findings to human application encompasses formidable hurdles. Efficient microglial targeting, immunocompatibility of donor cells, the long-term integration and function of replacement microglia, and potential off-target effects warrant extensive investigation. Future studies must also elucidate whether the benefits observed arise purely from enzymatic action or through complex modulatory interactions between microglia and neurons, including alterations in inflammatory milieu, synaptic stability, and metabolic homeostasis.
This study is distinguished not only by its clinical relevance but also by the sophisticated exploitation of modern genetic tools and cell biology insights. The Cre-Lox system enabled precise microglial ablation, while advanced imaging and biochemical assays quantified enzyme activity and ganglioside clearance at an unprecedented resolution. Behavioral tests, spanning grip strength measurements to coordinated movement assessments, complemented molecular findings with functional endpoints, thereby painting a comprehensive portrait of disease amelioration.
Crucially, the work also contributes to an evolving understanding of microglial heterogeneity and plasticity. The donor microglia, derived from wild-type mice, adapted to the Sandhoff brain environment, likely shifting their transcriptomic profiles in response to local cues. Understanding this adaptability may illuminate how microglia can be manipulated or reprogrammed therapeutically in diverse contexts beyond lysosomal diseases, including Alzheimer’s or Parkinson’s disease.
Beyond therapeutic perspectives, these results deepen our fundamental grasp of brain biology. The recognition that myeloid cells operating within the central nervous system produce and supply essential enzymatic functions blurs traditional boundaries between immune cells and neurons. It compels reconsideration of how intercellular cooperation maintains homeostasis and how disruptions trigger neurodegeneration. Such insights resonate with emerging views of the brain as a dynamically interactive multicellular community rather than an assembly of isolated neuron-centric circuits.
In conclusion, the study by Tsourmas et al. represents a landmark advance elucidating the indispensable contribution of microglial β-hexosaminidase to neuronal health in Sandhoff disease. Their innovative microglial replacement model not only reveals a causal therapeutic target but also stimulates broader reflections on the intersections of neuroimmunology, enzymology, and cell therapy. As this research propels the field forward, it offers hope for developing transformative treatments that might one day halt or reverse the dreadful course of lysosomal neurodegenerative diseases. With careful translation and continued exploration, immune cell-mediated enzyme restitution could emerge as a pillar of next-generation neurotherapeutics, exemplifying the power of harnessing the brain’s own cellular collaborators.
Subject of Research: Microglial contribution to neuronal health in Sandhoff disease through β-hexosaminidase enzyme activity.
Article Title: Microglial replacement in a Sandhoff disease mouse model reveals myeloid-derived β-hexosaminidase is necessary for neuronal health.
Article References:
Tsourmas, K.I., Butler, C.A., Kwang, N.E. et al. Microglial replacement in a Sandhoff disease mouse model reveals myeloid-derived β-hexosaminidase is necessary for neuronal health. Nat Commun 16, 7994 (2025). https://doi.org/10.1038/s41467-025-63237-0
Image Credits: AI Generated