In the ever-evolving landscape of cancer research, a groundbreaking discovery has emerged from a recent study that sheds light on a molecular mechanism driving resistance to immunotherapy in hepatocellular carcinoma (HCC). Published in Nature Communications, the research led by Lei et al. uncovers the pivotal role of wild-type KRAS activation in facilitating tumor evasion of the immune response, specifically by undermining interferon-mediated immunity. This insight opens new vistas for understanding why certain liver cancers resist the transformative potential of immune checkpoint inhibitors, an advance that could shape future therapeutic strategies.
Hepatocellular carcinoma remains one of the most challenging cancers worldwide, with poor prognostic outcomes partly due to its immunosuppressive microenvironment and limited response to conventional treatments. Immunotherapies targeting immune checkpoints have revolutionized oncology but exhibit variable efficacy in HCC patients. The molecular underpinnings of this variability have been elusive. Lei and colleagues systematically investigated how the activation state of KRAS, a well-known oncogene commonly mutated in various cancers, influences the immune dynamics within HCC tumors, despite being in its wild-type form.
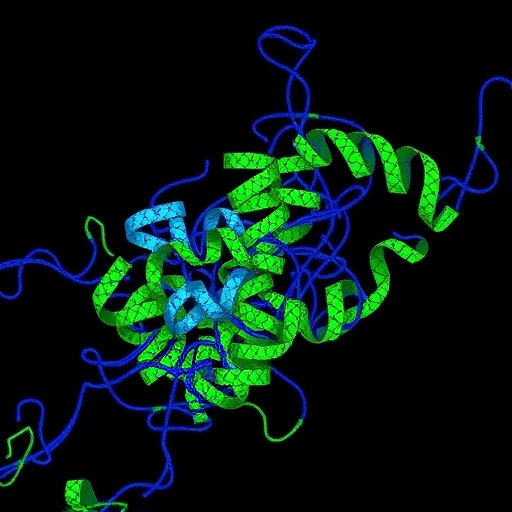
The study delineates a previously unappreciated role for wild-type KRAS, emphasizing that its activation—not mutation—is sufficient to elicit profound changes in the tumor immune milieu. By employing a combination of in vitro cell line models, patient-derived xenografts, and transcriptomic profiling, the researchers demonstrated that activated wild-type KRAS drives a robust suppression of interferon signaling pathways. The interferon pathway is crucial for eliciting an effective anti-tumor immune response, notably by promoting antigen presentation and the recruitment of cytotoxic immune cells.
Their analysis revealed that wild-type KRAS activation downregulates the expression of interferon-stimulated genes (ISGs), thereby blunting the tumor’s susceptibility to immune attack. This suppression extends to both type I and type II interferon responses, suggesting a broad-spectrum immune escapism strategy. The molecular crosstalk between KRAS signaling and interferon pathways was substantiated through phosphoproteomic analyses, which identified downstream signaling nodes potentially mediating this immune resistance phenomenon.
Beyond the molecular crosstalk, the study highlights the functional consequences of KRAS-induced immune evasion in the context of immunotherapy. When subjected to checkpoint blockade inhibitors targeting PD-1/PD-L1, models exhibiting wild-type KRAS activation demonstrated significantly impaired therapeutic responses. This finding suggests that KRAS activation status may serve as a predictive biomarker for resistance to immunotherapy, a revelation that demands clinical validation in patient cohorts.
The authors also explored therapeutic interventions that could potentially circumvent KRAS-driven immune evasion. Combining MEK inhibitors, which dampen KRAS downstream signaling, with immunotherapy restored interferon responsiveness and enhanced tumor control in experimental models. This combinatorial approach emphasizes the therapeutic synergy achievable through targeted molecular inhibition alongside immune checkpoint blockade.
Notably, the study’s implications extend to the broader understanding of oncogenic signaling pathways co-opting immune escape mechanisms. While mutant KRAS has been extensively studied for its oncogenic capacity, this research underscores that even the wild-type protein, when aberrantly activated, can reprogram the tumor microenvironment to its advantage. This paradigm shift challenges existing dogma and calls for a reassessment of KRAS’s role across different cancer types and treatment contexts.
From a translational perspective, the insights provided by Lei and colleagues could catalyze the development of precision immuno-oncology strategies tailored to the signaling landscape of tumors. Diagnostic assays assessing KRAS activation alongside interferon pathway status may help stratify patients for personalized interventions, optimizing clinical outcomes. Furthermore, targeting wild-type KRAS-induced immune modulation could help overcome one of the major barriers to effective immunotherapy in HCC.
Given the complexity of tumor-immune interactions, the elucidation of KRAS’s immunomodulatory function enriches our comprehension of tumor biology and reveals new therapeutic vulnerabilities. Importantly, the correlation between KRAS activation and immune suppression is likely influenced by a constellation of other factors, including tumor heterogeneity and microenvironmental cues, warranting deeper mechanistic explorations in future studies.
This seminal work adds a crucial layer to the fundamental narrative of cancer immune evasion and resistance mechanisms. It invites oncologists and researchers alike to consider the non-mutational activation of oncogenes as a critical determinant of tumor immune phenotypes. Consequently, therapeutic regimens that concurrently target oncogenic signaling and restore interferon responsiveness could become the cornerstone of next-generation immunotherapies.
In conclusion, the discovery that wild-type KRAS activation subverts interferon-mediated immunity marks a significant milestone in hepatocellular carcinoma research. It not only deepens our understanding of the molecular interplay between oncogenic drivers and immune escape but also highlights actionable targets to augment immunotherapeutic efficacy. As immunotherapy continues to reshape the cancer treatment paradigm, integrating such molecular insights will be paramount in overcoming resistance and improving patient survival.
This research opens the door to a new chapter where the nuanced roles of canonical oncogenes are revisited in the context of immune regulation. The potential to revert immune suppression by intercepting wild-type KRAS signaling offers hope for more effective treatments against a notably refractory cancer type. Ultimately, these findings underscore the intricate dance between tumor genetics and immune surveillance that defines therapeutic success.
Future research directions inspired by this work will likely focus on validating these findings in large clinical cohorts and expanding the therapeutic arsenal against KRAS-driven immune evasion. Investigations into whether similar mechanisms operate in other cancers or involve additional oncogenes could further revolutionize the field of cancer immunotherapy. The promise of converting immunologically “cold” tumors into “hot” ones by targeting wild-type KRAS activation is an exciting prospect that holds considerable translational promise.
As the oncology community grapples with the challenges of resistance to immunotherapies, studies like this exemplify the power of molecular biology to unravel hidden resistance pathways. By bridging oncogenic signaling with immune regulation, the scientific and medical communities are better equipped to devise integrated treatment strategies that anticipate and overcome tumor defenses.
Lei et al.’s landmark study is a testament to the critical importance of dissecting tumor biology at a granular level to unlock new avenues for effective cancer treatment. Harnessing this knowledge to inform clinical practice will be a pivotal step toward achieving durable remissions and ultimately cures for hepatocellular carcinoma patients worldwide.
Subject of Research: Mechanisms of immune evasion and therapeutic resistance in hepatocellular carcinoma mediated by wild-type KRAS activation.
Article Title: Wild-type KRAS activation drives evasion of interferon-mediated immunity and resistance to immunotherapy in hepatocellular carcinoma.
Article References:
Lei, M.M.L., Leung, C.O.N., Leung, R.W.H. et al. Wild-type KRAS activation drives evasion of interferon-mediated immunity and resistance to immunotherapy in hepatocellular carcinoma. Nat Commun 16, 9913 (2025). https://doi.org/10.1038/s41467-025-64860-7
Image Credits: AI Generated