In the relentless quest to unravel the complex mechanisms underlying glioblastoma—the most aggressive and lethal form of brain cancer—new research has spotlighted a critical molecular interplay that fuels tumor progression and stemness. A recent breakthrough study has identified the enzyme USP18 as a pivotal regulator that deubiquitinates and stabilizes the transcription factor SOX9, thereby sustaining the malignant traits and resilience of glioblastoma cells. This discovery not only broadens our understanding of glioblastoma biology but also opens promising avenues for targeted therapeutic interventions that could potentially undermine the tumor’s notorious resistance to conventional treatments.
Glioblastoma is characterized by its remarkable heterogeneity, aggressive invasion into surrounding brain tissue, and an uncanny ability to evade existing therapies, leading to dismal patient prognoses. Central to this malignancy is a subpopulation of cancer stem-like cells that drive tumor recurrence and therapeutic resistance. SOX9, a transcription factor well-known for its roles in development and stem cell biology, has emerged as a key player in maintaining this stem-like state. However, the post-translational dynamics that govern SOX9 stability within glioblastoma cells were poorly understood until now.
The study elucidates how USP18, a ubiquitin-specific protease, functions as a deubiquitinase for SOX9, effectively rescuing it from proteasomal degradation. Ubiquitination is a cellular process that tags proteins for destruction; in contrast, deubiquitination removes these tags, rescuing proteins from being broken down. By stabilizing SOX9, USP18 ensures the persistence of its oncogenic functions, such as promoting self-renewal, proliferative capacity, and survival of glioblastoma stem-like cells. This molecular axis thus represents a critical node in the maintenance of glioblastoma’s aggressive phenotype.
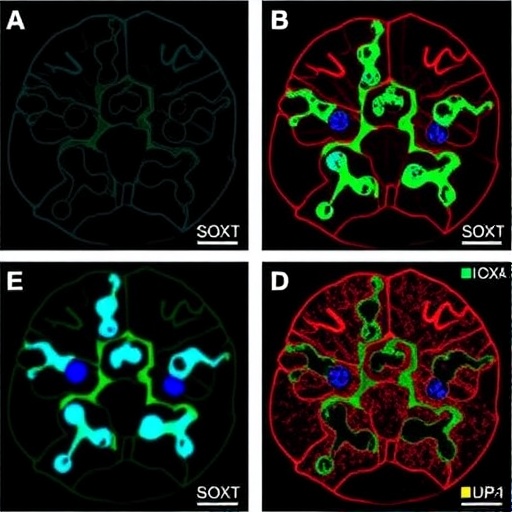
The researchers employed a combination of biochemical analyses, genetic manipulation, and in vitro and in vivo models to dissect the role of USP18 in glioblastoma. They demonstrated that knocking down USP18 leads to increased ubiquitination and subsequent degradation of SOX9, thereby impairing the stemness and proliferation of glioblastoma cells. Conversely, USP18 overexpression stabilized SOX9 and enhanced malignant properties, confirming the enzyme’s oncogenic influence. These manipulations directly impacted tumor growth rates and invasion capabilities in animal models, underscoring the clinical relevance of the findings.
Mechanistically, the deubiquitination activity of USP18 targets specific lysine residues on SOX9, preventing proteasome-mediated destruction. This direct interaction was confirmed through co-immunoprecipitation and ubiquitination assays, pinpointing USP18 as an indispensable regulator of SOX9 protein homeostasis. The stabilization of SOX9 consequently sustains the gene expression programs vital for glioblastoma stemness, including the regulation of pathways involved in cell cycle progression, survival, and DNA damage response.
Beyond the molecular interaction, the study sheds light on the broader oncogenic landscape of glioblastoma. The USP18-SOX9 axis represents a critical link connecting post-translational modification machinery to transcriptional control mechanisms sustaining tumor aggressiveness. Given the notorious difficulty in targeting transcription factors like SOX9 directly, USP18 emerges as an attractive druggable target. Inhibiting USP18’s enzymatic activity could destabilize SOX9, thereby attenuating the tumor’s stem cell-like properties and sensitizing glioblastoma cells to chemotherapy and radiotherapy.
Importantly, USP18 has been previously implicated in immune regulation and interferon signaling, indicating potential pleiotropic effects of targeting this protease. This dual functionality necessitates a nuanced therapeutic approach, possibly involving USP18 inhibitors tailored to selectively disrupt its interaction with SOX9 without compromising essential immune functions. The study’s insights into the specificity of USP18’s substrate interactions provide a valuable foundation for designing such targeted inhibitors.
In addition to therapeutic implications, this discovery advances the fundamental biology of glioblastoma by highlighting how protein stability regulation intricately controls cancer stem cell phenotypes. The ability of USP18 to modulate SOX9 protein levels post-translationally exemplifies the complex regulatory networks cancer cells leverage to maintain their malignant features. This underscores an emerging theme in oncology where deubiquitinases play central roles in sustaining oncogenic signaling pathways.
Further exploration of the USP18-SOX9 axis revealed that this interaction is dynamically regulated in response to environmental stressors and therapeutic pressures. For instance, hypoxic conditions within the tumor microenvironment and exposure to genotoxic agents appear to enhance USP18 expression, thereby reinforcing SOX9 stabilization and contributing to therapy resistance. Understanding these adaptive responses could inform the timing and combination of USP18-targeted therapies to maximize clinical efficacy.
Moreover, the spatial and temporal expression patterns of USP18 and SOX9 were characterized in glioblastoma patient samples, correlating high levels of both proteins with poorer clinical outcomes. This clinical correlation strengthens the translational relevance and positions USP18-SOX9 as a prognostic biomarker axis. Consequently, assessing USP18 and SOX9 expression could guide patient stratification and personalized treatment regimens designed to inhibit this malignant circuitry.
This landmark study expands the therapeutic horizon for glioblastoma by highlighting a novel vulnerability in the cancer’s molecular armor. Targeting the USP18-mediated stabilization of SOX9 presents a compelling strategy to dismantle the self-renewing tumor cell compartment that drives recurrence and resistance. As glioblastoma continues to defy conventional therapies, such innovative molecular insights offer a beacon of hope for developing more effective treatments and improving patient survival.
Future research directions will focus on developing small-molecule inhibitors or biologics that disrupt USP18’s catalytic function or its binding interface with SOX9. Additionally, integrating USP18 targeting with existing modalities, such as immune checkpoint blockade and radiotherapy, may produce synergistic effects. Combining these approaches could help overcome the multifaceted defense mechanisms glioblastoma employs, ushering in a new era of precision oncology tailored to the disease’s molecular underpinnings.
In conclusion, the study’s identification of USP18 as a master regulator of SOX9 stability and glioblastoma stemness represents a profound leap forward in understanding the disease’s biology. It exemplifies how deciphering post-translational modifications can reveal hidden drivers of tumor aggressiveness and resistance. With USP18’s enzymatic activity acting as a linchpin in maintaining the malignant phenotype, targeted interventions disrupting this axis hold transformative potential for combating glioblastoma’s devastating impact.
Subject of Research: Regulation of glioblastoma stemness and malignancy via USP18-mediated deubiquitination and stabilization of SOX9.
Article Title: USP18 deubiquitinates and stabilizes SOX9 to promote the stemness and malignant progression of glioblastoma.
Article References:
Liu, Z., Yu, K., Chen, K. et al. USP18 deubiquitinates and stabilizes SOX9 to promote the stemness and malignant progression of glioblastoma. Cell Death Discov. 11, 237 (2025). https://doi.org/10.1038/s41420-025-02522-9
Image Credits: AI Generated