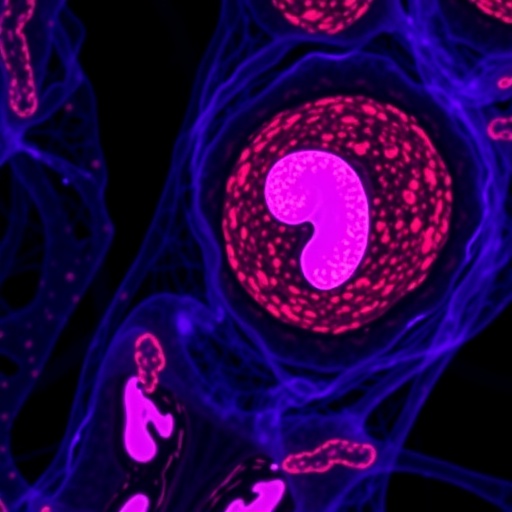
Recent advances in cancer research have highlighted the critical role of mitochondrial signaling in tumor progression, particularly through the intricate crosstalk between neutrophils and tumor cells. A groundbreaking study led by Shen, Pan, and Li et al., delves deep into the mechanisms by which neutrophils interact with cancer cells, potentially shaping the tumor microenvironment and influencing metastatic behavior. This research not only reveals the underlying complexity of immune cell-tumor interactions but also proposes new avenues for therapeutic interventions targeting these molecular pathways.
The mitochondrion, often dubbed the powerhouse of the cell, is not merely a site for energy production; it also serves as a signaling hub that affects various cellular processes. Recent studies have expanded our understanding of how mitochondrial dynamics, including changes in morphology and function, can impact immune responses. This work posits that alterations in mitochondrial signaling within neutrophils can modulate their behavior and, subsequently, their interactions with cancer cells.
In particular, the study presented by Shen et al. provides compelling evidence that mitochondrial signaling pathways are reprogrammed in neutrophils as they enter the tumor microenvironment. This reprogramming plays a pivotal role in influencing neutrophil activation, survival, and the release of pro-inflammatory mediators. These factors can create a feedback loop that further enhances the growth and invasiveness of cancer cells, underscoring the significance of these cellular interactions in tumor biology.
One of the fascinating findings reported in the study is the role of reactive oxygen species (ROS) produced by neutrophils in shaping the fate of tumor cells. The authors demonstrate that neutrophil-derived ROS can induce oxidative stress in cancer cells, potentially leading to their death or altered signaling within the tumor microenvironment. However, the study also reveals how cancer cells can exploit this ROS signaling to adapt and thrive, showcasing the dual nature of this interplay.
Furthermore, Shen et al. investigate the impact of various cytokines released by tumor cells on neutrophil behavior. The research outlines how factors such as IL-6, IL-8, and TNF-α can modulate neutrophil recruitment and function, establishing a communication network between the two cell types. This cytokine-mediated signaling is crucial for maintaining a pro-tumorigenic environment, reinforcing the importance of understanding these molecular interactions for potential therapeutic strategies.
As the study illustrates, the crosstalk between neutrophils and tumor cells does not occur in isolation. Instead, it is intricately linked to the broader immune landscape. The authors highlight how other immune cells, such as macrophages and T-cells, also participate in this complex network. The interplay among these various cell types can ultimately dictate the outcomes of cancer progression and therapy, making it essential to consider these interactions when designing clinical interventions.
In addition to exploring the molecular underpinnings of neutrophil-tumor cell interactions, the study also addresses potential therapeutic implications. By understanding how mitochondrial signaling affects the behavior of neutrophils in tumors, researchers can discover novel targets for drug development. For instance, modulating mitochondrial dynamics or targeting specific metabolic pathways within neutrophils may offer new methods to enhance tumor targeting and improve patient outcomes.
Moreover, the findings from this research open new doors for combination therapies. By integrating mitochondrial-targeting agents with existing immunotherapies, there is potential to augment the efficacy of treatments while also minimizing adverse effects. This idea of synergistic therapies could represent a paradigm shift in how we approach cancer treatment, emphasizing the need for more personalized strategies that take into account the unique characteristics of each patient’s tumor microenvironment.
The implications of this research extend beyond the realm of basic science. It holds promise for clinical applications, particularly in understanding treatment resistance mechanisms. Many tumors exhibit resilience against therapies, in part due to the support from immune cells like neutrophils. By dissecting the role of mitochondrial signaling in these interactions, clinicians may develop better strategies to overcome resistance and improve treatment efficacy.
Furthermore, as we fundamentally rethink our approach to cancer biology, the study encourages us to challenge existing paradigms. The current focus has heavily been on tumor-intrinsic factors; however, this work compels us to consider how extrinsic factors, particularly from the immune system, actively shape tumor development and therapeutic responses. Such an integrated view could foster innovative strategies for early detection, prognosis, and treatment.
In conclusion, Shen, Pan, and Li et al. provide a significant contribution to the understanding of the complex interactions between neutrophils and tumor cells through mitochondrial signaling. This research emphasizes that modulating these interactions may represent a viable strategy to combat cancer progression. Future studies should aim to further elucidate the precise mechanisms involved, paving the way for novel therapeutic avenues that hold the potential to transform cancer treatment as we know it.
The study not only advances our scientific knowledge but serves as a reminder of the intricacies of cancer biology, where immune cells, signaling pathways, and tumor dynamics converge. As this field continues to evolve, the insights gained from such research will undoubtedly shape the next generation of oncology, with the goal of improving patient outcomes in the ongoing fight against cancer.
By exploring the nuances of neutrophil-tumor cell interactions, we are better equipped to understand the multifaceted nature of cancer biology and the role of the immune system, making strides toward developing more effective treatments that significantly impact patient lives.
In summary, the discovery that mitochondrial signaling plays a vital role in the crosstalk between neutrophils and tumor cells opens new pathways for cancer research and therapeutics. With further exploration and technological innovation, we anticipate that researchers will uncover additional layers of complexity within this interaction, ultimately leading to breakthroughs that will benefit countless patients battling cancer.
Subject of Research: Mitochondrial signaling in neutrophil-tumor cell interactions and cancer progression.
Article Title: Decoding mitochondrial signaling: neutrophil-tumor cell crosstalk in orchestrating cancer progression.
Article References:
Shen, Q., Pan, X., Li, J. et al. Decoding mitochondrial signaling: neutrophil-tumor cell crosstalk in orchestrating cancer progression.
J Transl Med (2026). https://doi.org/10.1186/s12967-025-07659-w
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07659-w
Keywords: mitochondrial signaling, neutrophil-tumor cell interaction, cancer progression, immune response, therapeutic implications.