In the relentless battle against cancer, acute myeloid leukemia (AML) remains one of the most aggressive and enigmatic foes in hematological oncology. Recent advances, however, have unveiled a more detailed map of this malignancy’s molecular underpinnings, leveraging cutting-edge systems biology approaches to chart the initiation and relapse pathways of the disease. A groundbreaking study led by Bahmei, Fadakar, and Tamaddon, published in Medical Oncology in 2025, dives deep into the intricate molecular choreography that governs AML, offering new hope for innovative therapeutic strategies and relapse prevention.
Acute myeloid leukemia is characterized by a rapid proliferation of abnormal myeloid progenitor cells in the bone marrow, which crowd out healthy blood cells and quickly lead to bone marrow failure and systemic complications. Despite intensive chemotherapy and bone marrow transplantation, relapse rates remain distressingly high, with survival statistics stagnating for decades. Understanding the molecular events that drive both the initiation of AML and its recurrence after therapy is thus crucial—not only to develop precise treatment regimens but to potentially anticipate and preempt relapse.
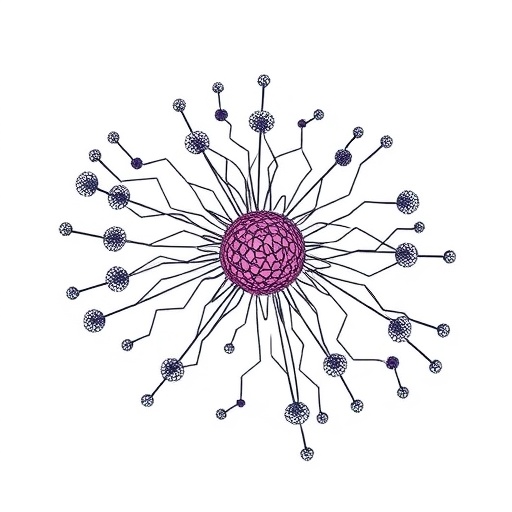
The study employs a systems biology framework, a discipline that integrates complex biological data through computational modeling and network analysis. By examining gene expression profiles, epigenetic modifications, signaling cascades, and cellular interactions as interconnected elements rather than isolated events, the researchers paint a comprehensive picture of AML’s molecular landscape. This holistic vantage point allows for identification of crucial regulatory nodes and pathways that may serve as master regulators of leukemogenesis and resistance mechanisms.
One of the pivotal findings of the investigation is the delineation of a core gene regulatory network that governs stemness and differentiation in hematopoietic cells. Leukemic stem cells (LSCs), the root of AML initiation and persistence, exhibit aberrant activation of transcription factors and signaling pathways that sustain their self-renewal while blocking differentiation. Such dysregulation results in the unchecked growth and survival of malignant clones. Crucially, this regulatory topology is distinct from that in normal hematopoietic stem cells, highlighting specific therapeutic targets to selectively eradicate LSCs without harming healthy progenitor cells.
The study further unpacks the genetic and epigenetic heterogeneity that underscores AML relapse. Post-treatment relapse is not merely a result of residual disease; it reflects an evolutionary process in which leukemic cells acquire mutations and epigenetic changes that confer resistance to chemotherapy. By comparing molecular profiles from diagnosis and relapse samples, the researchers identified key alterations in DNA methylation patterns and chromatin remodeling factors that reshape gene expression landscapes, enabling leukemic clones to escape therapeutic eradication.
In parallel, the authors mapped the signaling networks modulated by microenvironmental cues within the bone marrow niche. Interactions between leukemic cells and stromal components were shown to induce protective signaling pathways such as NF-κB and PI3K/AKT, which promote survival and drug resistance. Understanding these extrinsic influences is essential for developing combination therapies that disrupt these protective niches, sensitizing leukemic cells to chemotherapy and immunotherapy.
Importantly, the systems biology approach revealed dynamic feedback loops within signaling and transcriptional networks that stabilize leukemic phenotypes. These feedback mechanisms maintain the delicate balance of cell proliferation, differentiation blockade, and survival signals, making them attractive nodes for pharmacological intervention. Targeting these loops could destabilize the leukemic state, forcing malignant cells into apoptosis or differentiation.
One of the most compelling aspects of this research is the use of integrative multi-omics data, combining genomics, transcriptomics, epigenomics, and proteomics, to achieve a robust system-level insight. This integration allows for prediction of functional consequences of molecular alterations and identification of novel biomarkers for early detection of relapse. High-resolution computational models generated in the study enable simulation of treatment responses, opening avenues for personalized medicine approaches in AML.
Furthermore, the study sheds light on the role of metabolic reprogramming in AML pathogenesis and relapse. Leukemic cells exhibit shifts in energy production and nutrient utilization, supporting anabolic growth and survival under stress conditions, including chemotherapy. Targeting metabolic vulnerabilities revealed through systems analysis could complement genetic and epigenetic targeting strategies, overcoming resistance and improving patient outcomes.
Clinical translation of these findings is already underway, with candidate molecules identified by network analysis being tested in preclinical models. The research not only underscores the complexity of AML as a disease of both genetic mutation and cellular circuitry but also provides a rational blueprint for combination therapies that address multiple layers of leukemic maintenance and evolution.
In conclusion, the molecular landscape of AML as described through this systems biology lens exposes a labyrinth of interconnected regulatory elements that drive disease initiation and relapse. Through dissecting these networks, Bahmei, Fadakar, and Tamaddon have contributed seminal insights that elevate our understanding of leukemia biology to unprecedented depths. Their work lays a foundation for innovative interventions capable of eradicating residual disease and preventing relapse, ultimately transforming the paradigm of AML treatment.
The integration of computational modeling with empirical data exemplifies a new era in oncology research, where big data and systems thinking converge to solve the intricate puzzles of cancer progression. This approach is poised to redefine how we conceptualize not only leukemia but cancer in general—highlighting the power of comprehensive network analysis in identifying elusive therapeutic targets beyond single-gene effects.
As research progresses, further refinement in system models and real-time monitoring of molecular dynamics in patients could lead to adaptive therapies that evolve in response to tumor changes, much like a responsive immune system. Such innovations will be essential in combating the adaptability and resilience of AML, ultimately improving survival and quality of life for patients worldwide.
Undoubtedly, this study marks a significant stride forward in leukemia research, exemplifying the transformative impact of systems biology on understanding complex diseases. By illuminating the multifaceted mechanisms behind AML initiation and relapse, the work inspires hope for more durable remissions and, eventually, cures.
Subject of Research: Acute Myeloid Leukemia molecular mechanisms of initiation and relapse through systems biology analysis.
Article Title: Deciphering the molecular landscape of acute myeloid leukemia initiation and relapse: a systems biology approach.
Article References:
Bahmei, A., Fadakar, H. & Tamaddon, G. Deciphering the molecular landscape of acute myeloid leukemia initiation and relapse: a systems biology approach. Med Oncol 42, 468 (2025). https://doi.org/10.1007/s12032-025-03003-w
Image Credits: AI Generated