Recent advances in the field of oncology have brought to light novel treatment strategies for patients suffering from hepatocellular carcinoma (HCC), particularly those with a high tumor burden. A groundbreaking study led by Lin et al. examines the efficacy of combining tyrosine kinase inhibitors (TKIs) with immune checkpoint inhibitors (ICIs) in comparison to the use of ICIs alone. This retrospective cohort study represents an essential step in understanding potential therapeutic benefits for patients with advanced stages of this malignancy.
Hepatocellular carcinoma is a primary liver cancer that ranks among the leading causes of cancer-related deaths globally. Current treatment options for high tumor burden cases are limited and often unsatisfactory. The need for innovative therapeutic strategies is pressing, as patients often present with advanced disease where curative interventions are no longer feasible. In this context, the integration of immunotherapy and targeted therapy could offer new avenues for managing this aggressive cancer.
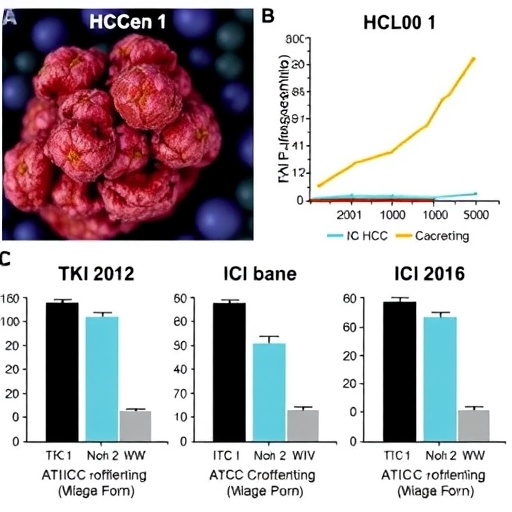
The study focuses on the dynamics between TKIs and ICIs, two classes of medications that have gained traction in the treatment of various cancers over recent years. TKIs are designed to inhibit specific pathways that facilitate cancer growth and metastasis, while ICIs work by unleashing the body’s immune system against cancer cells. When these two classes are used in conjunction, there is reason to believe that a synergistic effect could enhance anti-tumor responses.
To evaluate the effectiveness of this combination therapy, the researchers analyzed clinical data from a cohort of patients with high tumor burden HCC. They compared the outcomes of those receiving the combined treatment (TKI plus ICI) to those treated with ICI alone. The results proved significant and suggest that the combination may lead to improved survival rates for these patients. Specifically, the reduced tumor size and improved response rates highlight the potential of this therapeutic strategy.
The study also underscores the importance of patient selection when considering combination therapies. Not all patients may benefit equally from dual treatment approaches. Factors such as tumor characteristics, genetic markers, and overall health status can influence the outcomes significantly. The retrospective nature of the study necessitates further validation through prospective trials to confirm these findings and refine patient selection criteria.
Moreover, the implications of this research extend beyond survival rates. Quality of life, treatment side effects, and overall patient experience are critical considerations in the treatment of HCC. Integrating a multi-faceted treatment approach can potentially enhance not just the survival of patients but also the quality of life, as effective therapies typically lead to better management of symptoms associated with advanced liver cancer.
The exploration of TKIs and ICIs is not solely confined to HCC; it has broader implications for oncology as a whole. As researchers continue to explore the synergistic potential of combining different therapeutic modalities, there is hope for patients with other types of tumors facing similar challenges. The results from Lin et al. could serve as a template for future studies in other cancers, paving pathways for effective combination therapies.
Despite the promising findings, the study is not without its limitations. The retrospective nature means the data could be subject to biases or confounding variables. However, the study opens exciting avenues for future research, including multi-center prospective trials and molecular profiling studies to identify which patients are most likely to benefit from TKIs combined with ICIs.
In conclusion, the research by Lin et al. highlights a significant advancement in the treatment landscape for high tumor burden hepatocellular carcinoma. The combination of TKIs and ICIs may redefine therapeutic strategies in managing this challenging cancer. As researchers continue to unravel the complexities of tumor biology and patient responses to therapies, the hope for more effective treatments becomes increasingly tangible. This work not only contributes to the scientific community’s understanding of HCC but also emphasizes the importance of innovative, personalized treatment approaches in oncology.
As we look to the future, it is vital to continue supporting and funding research that explores the intricacies of cancer mechanisms and treatment efficacy. The potential for breakthroughs in managing high tumor burden HCC and other malignancies holds promise, and it is an area worthy of close attention from both the scientific community and cancer care advocates. The findings from this study could be a catalyst for change, leading to more effective therapeutic strategies tailored to individual patients.
In an era where precision medicine is becoming increasingly prominent, studies like this remind us of the importance of integrating various treatment modalities to create a holistic approach to cancer care. As the field evolves, so too must our strategies and understanding, ensuring that we not only strive for survival but also for the enhancement of patient wellness throughout their cancer journey.
Subject of Research: Combination Therapy in High Tumor Burden Hepatocellular Carcinoma
Article Title: TKI plus ICI versus ICI alone in high tumor burden hepatocellular carcinoma: a retrospective cohort study
Article References: Lin, PT., Teng, W., Chen, WT. et al. TKI plus ICI versus ICI alone in high tumor burden hepatocellular carcinoma: a retrospective cohort study. J Cancer Res Clin Oncol 152, 4 (2026). https://doi.org/10.1007/s00432-025-06381-w
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00432-025-06381-w
Keywords: Hepatocellular carcinoma, tyrosine kinase inhibitors, immune checkpoint inhibitors, cancer therapy, combination treatment, patient outcomes.