In the realm of pediatric oncology, the emergence of rhabdoid tumors has been a subject of increasing concern among healthcare professionals. These tumors, known for their aggressive behavior and tendency to exhibit a diverse array of clinical presentations, challenge both diagnosis and management strategies. Recent studies have focused not just on the primary tumors, but also on their associated complications, such as subcapsular effusions. This particular feature, as highlighted in groundbreaking research, underscores the complex nature of pediatric renal rhabdoid tumors.
Subcapsular effusions present a clinical enigma. They often arise as a consequence of underlying disease processes, prompting healthcare teams to delve into the intricacies of renal pathology. The presence of fluid collections near the renal capsule can signify various phenomena, from inflammatory responses to direct tumor involvement. However, the existing literature has only scratched the surface of our understanding of this intricate association. Thus, investigations into cases of subcapsular effusion in pediatric renal rhabdoid tumors are paramount to improving outcomes.
In a significant contribution to this discourse, the work of Dawa et al. brings new insights into the nature of subcapsular effusions associated with rhabdoid tumors in children. The research meticulously describes the occurrence of these effusions, emphasizing that while they are not unique to rhabdoid tumors, their presence in this context often indicates a more severe underlying pathological state. These findings have exciting implications, as they may help clinicians anticipate potential complications, tailor treatment strategies, and ultimately enhance patient care.
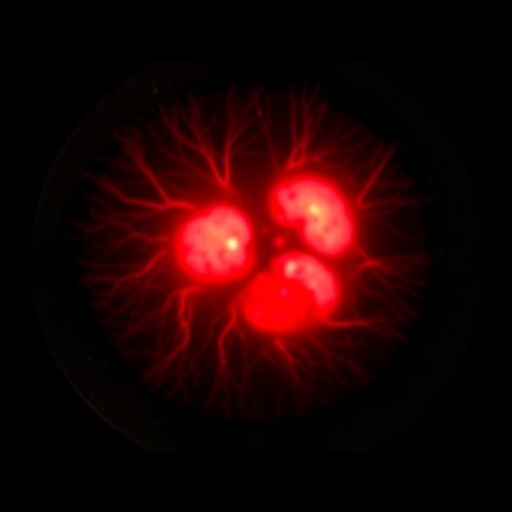
From a diagnostic standpoint, the challenge remains to differentiate between benign and malignant causes of subcapsular effusions. In the pediatric population, characterized by anatomical and physiological differences, the interpretation of imaging studies can be particularly challenging. Dawa et al. illuminate the nuances involved in using imaging techniques, such as ultrasound and magnetic resonance imaging (MRI), to identify subcapsular effusions in this patient demographic. These visualizations not only assist in diagnosis but can also guide surgical intervention, where necessary.
The authors’ exploration into the biological underpinnings of rhabdoid tumors complements their clinical observations. By delving into the pathophysiology behind the tumor’s behavior, they provide a comprehensive overview that may enhance our interpretation of associated presentations like subcapsular effusion. Rhabdoid tumors are notable for their loss of function mutations in the SMARCB1 gene, which results in disruptions to chromatin remodeling. This genetic alteration can lead to varying tumors’ microenvironments, characterized by inflammatory cell infiltrates and vascular changes that may contribute to fluid accumulation.
Equally important is the research’s exploration of therapeutic implications. As treatments for rhabdoid tumors evolve, understanding the implications of subcapsular effusions on treatment plans becomes critical. For instance, patients presenting with significant effusion may require alterations in their surgical approach or a more aggressive systemic therapy regimen. The article emphasizes that early recognition and management of such effusions could potentially enhance treatment efficacy and promote better prognostic outcomes.
The study also urges further research into the management protocols for these effusions, particularly in the context of fluid drainage options versus conservative monitoring. With advancements in minimally invasive techniques, such as ultrasound-guided drainage, pediatric oncologists may have additional tools to optimize care for these complex cases. The multifactorial considerations influencing treatment decisions for subcapsular effusions in the context of rhabdoid tumors underscore the need for a personalized approach.
Moreover, the psychological impact of pediatric tumors on families cannot be overlooked. The challenges posed by a child’s diagnosis of a rhabdoid tumor extend beyond physical manifestations, affecting emotional and mental health as well. Understanding complications like subcapsular effusions can alleviate some anxieties for families by providing a clearer picture of potential treatment pathways, even in the face of uncertainty. Education and transparent communication become paramount in the holistic care of these patients.
As research continues to unfold in the field of pediatric oncology, it is imperative for the medical community to engage in dialogue regarding cases of subcapsular effusion and their implications. Collaborative discussions among oncologists, radiologists, and pathologists can pave the way for deeper understanding and improved management strategies. The importance of sharing insights and experiences related to subcapsular effusion in pediatric renal rhabdoid tumors cannot be understated in our collective pursuit of advancing patient care.
Furthermore, the global focus on pediatric cancers has inspired a new wave of research initiatives aimed at understanding these complex pathologies. Funding and support for comprehensive studies in this area remain crucial, as insights gained today can shape the future landscape of pediatric oncology. The juxtaposition of basic science and clinical application will ultimately drive the next generation of therapeutic advancements.
In conclusion, the findings outlined by Dawa et al. serve as a catalyst for deeper inquiry into the relationship between subcapsular effusions and rhabdoid tumors in children. Their efforts to shed light on this intricate association, coupled with their commitment to enhancing diagnostic accuracy and clinical outcomes, advance our understanding in this critical domain of pediatric medicine. The complexities associated with rhabdoid tumors demand sustained research efforts and collaboration, reiterating that continued investigation is paramount to achieving breakthroughs in pediatric oncology.
As healthcare professionals and researchers endeavor to unravel these complexities, their collective expertise will undoubtedly coalesce into a more robust understanding of the relationship between subcapsular effusions and pediatric renal rhabdoid tumors. This research not only contributes to the existing body of literature but also lays the groundwork for future explorations, hopefully leading to enhanced therapies and improved quality of life for young patients grappling with these challenging conditions.
Subject of Research: Subcapsular effusion in pediatric renal rhabdoid tumors
Article Title: Subcapsular effusion in a pediatric renal rhabdoid tumor
Article References:
Dawa, P., Wang, X., Gao, Q. et al. Subcapsular effusion in a pediatric renal rhabdoid tumor.
Pediatr Radiol (2025). https://doi.org/10.1007/s00247-025-06362-8
Image Credits: AI Generated
DOI: https://doi.org/10.1007/s00247-025-06362-8
Keywords: Pediatric oncology, rhabdoid tumor, subcapsular effusion, diagnosis, treatment, imaging, genetics, patient care.