In an exciting new study, researchers have unveiled critical insights into the mechanisms that underpin resistance to osimertinib, a targeted therapy used for treating non-small cell lung cancer (NSCLC) with EGFR mutations. The article emphasizes the role of PD-L1, a key immune checkpoint protein, in regulating c-MET phosphorylation, which has profound implications for patients battling this aggressive form of cancer. This research not only sheds light on the biological complexities of tumor resistance but also opens up potential therapeutic avenues that could enhance treatment efficacy for EGFR-mutant NSCLC.
Osimertinib represents a significant advancement in personalized cancer therapy, specifically designed to target the tyrosine kinase activity of mutated EGFR. However, resistance to this agent has emerged as a formidable challenge in clinical settings. This study highlights that one of the mechanisms through which resistance occurs involves the interaction between PD-L1 and c-MET signaling pathways. By dissecting these molecular interactions, the researchers have pinpointed a crucial axis that contributes to both resistance and tumor progression.
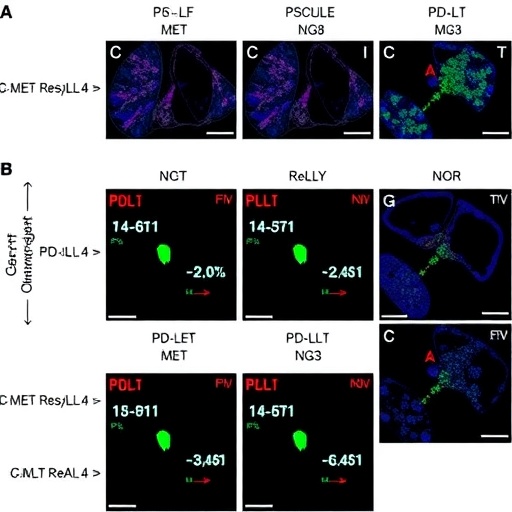
The study was conducted through a series of in vitro and in vivo experiments designed to explore the interplay between PD-L1 and c-MET. The researchers employed advanced techniques such as western blotting and immunoprecipitation to measure the phosphorylation status of c-MET in the presence of PD-L1. Through rigorous analysis, they found that PD-L1 not only modulates the phosphorylation of c-MET but also influences downstream signaling pathways that are pivotal for cell survival and proliferation, thereby allowing cancer cells to thrive even in the backdrop of targeted therapy.
An important takeaway from the findings is the pivotal role of the tumor microenvironment in creating a scaffold that promotes resistance. PD-L1, traditionally recognized for its role in suppressing T-cell activity and dampening immune responses, can enhance c-MET signaling under specific conditions. In the context of EGFR-mutant NSCLC, this creates a dual challenge: not only does the tumor evade immune detection, but it also activates pathways that bolster its survival against targeted therapies.
Moreover, the researchers found that high levels of PD-L1 in tumor samples correlated with increased c-MET phosphorylation, indicating that tumors with elevated PD-L1 expression may exhibit a heightened resistance to osimertinib. This correlation underscores the complexity of cancer biology, where a single protein can have multifaceted roles that significantly impact treatment outcomes. The implications of these findings could lead to a paradigm shift in how oncologists view PD-L1—not merely as a biomarker for immunotherapy but as a contributing factor to resistance mechanisms in mutant EGFR-driven tumors.
The researchers also performed a series of combination therapy trials to assess the potential of targeting both PD-L1 and c-MET concurrently. Preliminary results indicate that when osimertinib is combined with PD-L1 inhibitors, there is a marked improvement in the sensitivity of NSCLC cells to the treatment. This combination approach appears to disrupt the PD-L1/c-MET signaling axis, re-sensitizing tumors to osimertinib and overcoming the resistance that has plagued many patients.
In addition to providing critical insights into therapeutic resistance, the study calls for reevaluating the use of PD-L1 as a biomarker in treatment decisions. As oncologists strive to tailor therapies specifically to individual patients, understanding the nuances of PD-L1’s role in tumor biology could prove essential in predicting which patients may harbor a greater risk of resistance. If validated in clinical settings, the findings from this research could pave the way for more personalized, effective treatment plans for patients with EGFR-mutant NSCLC.
The study faced challenges that are typical in cancer research, including the heterogeneity of tumors and the complexity of signaling pathways. However, the rigorous methodologies employed, along with detailed analysis, provide a robust framework for understanding the role of PD-L1 in c-MET signaling. As ongoing research continues to unravel these intricacies, the potential to develop novel therapeutic strategies increases.
This research is expected to inspire further studies aimed at dissecting the complete molecular landscape of EGFR-mutant NSCLC. The team encourages collaboration across different research institutions to validate their findings and to test these insights in clinical trial settings. Such partnerships could accelerate the translation of laboratory findings into clinical practice, ultimately benefiting patients who currently face limited options.
In summary, the work highlights PD-L1 as a critical player in the resistance mechanisms associated with osimertinib therapy for EGFR-mutant NSCLC. By uncovering the link between PD-L1 and c-MET phosphorylation, the researchers have taken a significant step towards deciphering the complexities of cancer resistance. Future work in this direction may provide not only hope for enhanced therapeutic regimens but also a deeper understanding of the dynamic relationships at play in tumor biology.
As patients and clinicians grapple with the challenges that accompany treatment resistance, it is crucial to remain optimistic about the pathway forward. With each research endeavor, the aim is not solely to enhance existing treatments but also to foster innovation that could lead to new therapeutic fronts. This research marks a promising chapter in the ongoing battle against cancer and exemplifies the need for continued exploration into the crossroads of immunology and targeted therapies.
Ultimately, the findings from this study underscore a crucial juncture in our understanding of cancer therapies, emphasizing that an integrated approach that includes immune modulation may be key to overcoming resistance and improving patient outcomes. The journey toward effective cancer treatment is an evolving saga, and with each new discovery, hope is reawakened for patients worldwide.
Subject of Research: Resistance mechanisms in EGFR-mutant non-small cell lung cancer (NSCLC) related to PD-L1 and c-MET interaction.
Article Title: PD-L1 regulates c-MET phosphorylation and contributes to MET-dependent resistance to osimertinib in EGFR-mutant NSCLC.
Article References:
Hsu, CC., Huang, D.DR., Hsu, WH. et al. PD-L1 regulates c-MET phosphorylation and contributes to MET-dependent resistance to osimertinib in EGFR-mutant NSCLC.
J Biomed Sci 32, 94 (2025). https://doi.org/10.1186/s12929-025-01181-3
Image Credits: AI Generated
DOI: 10.1186/s12929-025-01181-3
Keywords: PD-L1, c-MET, osimertinib, EGFR-mutant NSCLC, resistance mechanisms.