Immune-checkpoint inhibitors (ICIs) have emerged as a transformative approach in the treatment landscape of various solid tumors. Among these, agents targeting programmed cell death 1 (PD1) and its ligand, programmed cell death 1 ligand 1 (PDL1), have been pivotal in revolutionizing patient care and enhancing survival rates across different malignancies. However, their efficacy in muscle-invasive bladder cancer (MIBC) remains disappointingly low, with studies indicating that only 20–30% of affected patients exhibit a sustained response to such therapies. This stark reality underscores an urgent need for deeper insights into the mechanisms driving resistance to ICIs in MIBC, which can ultimately guide the development of more effective treatment strategies.
A crucial area of research is the tumor microenvironment, particularly the role of hypoxia—a condition characterized by low oxygen tension—within MIBC. Hypoxic conditions are commonly observed in many solid tumors, including bladder cancer, and they significantly influence the behavior of various immune cells, particularly neutrophils. Recent findings point to a connection between hypoxia-driven extracellular matrix (ECM) remodeling and the polarization of neutrophils, which can either foster tumor growth or enhance anti-tumor immunity. Understanding how hypoxia modifies the ECM is vital, as it creates a complex interplay between tumor cells, ECM components, and immune effector cells that could contribute to ICI resistance.
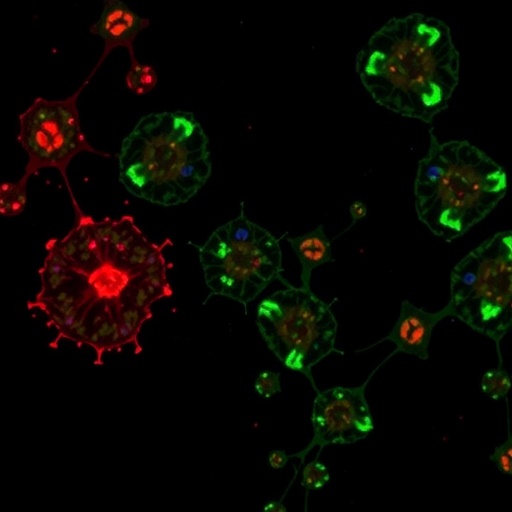
Neutrophils, known for their role in the innate immune response, are increasingly recognized as pivotal players in the tumor microenvironment. In MIBC, these cells can become polarized into distinct phenotypes that may either support tumor progression or combat malignancy. Hypoxia can dictate the behavior of neutrophils by influencing both their recruitment to the tumor site and their subsequent functional state. This duality of neutrophils—acting as both potential allies and adversaries in cancer progression—adds a layer of complexity to the understanding of ICI effectiveness in MIBC.
The mechanisms through which hypoxia and ECM dynamics interact to shape the immune landscape in tumors are not yet fully elucidated. Hypoxia can alter the composition and architecture of the ECM, which in turn can affect how neutrophils are recruited and activated. These changes could lead to a microenvironment that is more conducive to tumor growth, thereby helping the cancer evade immune detection. Furthermore, the shift in ECM properties may influence the mechanical forces experienced by immune cells, which can affect their behavior and efficacy in responding to therapeutic interventions.
Investigating the interplay between hypoxia, ECM remodeling, and neutrophil dynamics holds promise for developing novel strategies to overcome resistance to ICIs in MIBC. By identifying specific pathways associated with ECM alterations and neutrophil polarization, researchers could potentially create targeted interventions aimed at modifying the tumor microenvironment. Such approaches could enhance the efficacy of existing immunotherapies, potentially increasing the response rate from the current 20–30% to a more promising range of 70–80% for patients who are currently ineffective responders to ICIs.
By unraveling the intricate mechanisms that underpin immunotherapy resistance in MIBC, researchers could pave the way for personalized treatment modalities. This enhanced understanding could allow for the stratification of patients based on their ECM and immune profiles, leading to tailored therapeutic approaches that truly address the individual needs of each patient. The possibility of combining ICIs with modulators that specifically target the unfavorable features of the tumor microenvironment is tantalizing and could mark a significant step forward in improving outcomes for MIBC patients.
In light of these findings, there is an urgent call for further research to elucidate the specific pathways through which hypoxia, ECM remodeling, and neutrophil dynamics confer immunotherapy resistance. Translating preclinical insights into clinical applications will be paramount, as this knowledge will guide the design of innovative trials that test novel combination therapies. By combining immune-checkpoint blockade with agents that target hypoxic conditions or ECM components, clinicians may be able to elicit more durable and robust responses in a broader patient population.
Moreover, identification of reliable biomarkers reflective of hypoxic status and ECM alterations could serve as critical tools for predicting patient responses to ICIs. Such biomarkers might facilitate better patient stratification, ensuring that therapies are directed toward those most likely to benefit. As the field advances, integrating biomarker discovery alongside therapeutic innovation will be essential for maximizing the potential of immunotherapy in MIBC.
In summary, the landscape of immunotherapy in muscle-invasive bladder cancer is fraught with challenges related to resistance. Yet, the multifaceted interactions between hypoxia, ECM, and neutrophil responses hold significant promise for overcoming these barriers. As research continues to evolve, the hope is to unlock the full potential of immune-checkpoint inhibitors and transform MIBC into a more manageable condition, ultimately improving survival outcomes for patients grappling with this aggressive disease.
The interplay between biological and mechanical aspects in the tumor microenvironment is set to redefine the therapeutic horizon in bladder cancer. The clock is ticking, and the urgency to translate findings from laboratory to clinic is paramount, with the potential to set a new precedent in cancer treatment paradigms. The next chapters in this narrative will undoubtedly unfold new insights that could reshape the future of oncological therapeutics, making the dream of personalized cancer care a tangible reality for those affected by MIBC.
With ongoing research efforts focusing on these dynamic interactions, the medical community is on the brink of potentially groundbreaking advancements. The promise of enhancing the efficacy of immunotherapies in muscle-invasive bladder cancer through targeted manipulation of the tumor microenvironment is a beacon of hope that underscores the importance of continued investigation in this critical field.
Subject of Research: Mechanisms of Immunotherapy Resistance in Muscle-Invasive Bladder Cancer
Article Title: The hypoxic ECM and neutrophils in MIBC immunotherapy resistance
Article References:
Child, F., Lunj, S., Gough, J. et al. The hypoxic ECM and neutrophils in MIBC immunotherapy resistance.
Nat Rev Urol (2025). https://doi.org/10.1038/s41585-025-01092-w
Image Credits: AI Generated
DOI:
Keywords: Immunotherapy, Muscle-Invasive Bladder Cancer, Hypoxia, Neutrophils, ECM Remodeling, ICI Resistance.