In an era where mental health challenges are increasingly recognized as critical public health issues, the quest for reliable biomarkers that can predict treatment outcomes in suicidal ideation has become paramount. Recent advances in neurophysiology are shedding unprecedented light on this complex terrain, promising to revolutionize clinical approaches and patient outcomes. A newly published systematic review in Translational Psychiatry has embarked on a comprehensive exploration of neurophysiological biomarkers, meticulously analyzing their potential in forecasting treatment response among individuals grappling with suicidal thoughts. This review marks a significant milestone, offering a nuanced synthesis of cutting-edge research that bridges neuroscience, psychiatry, and clinical practice.
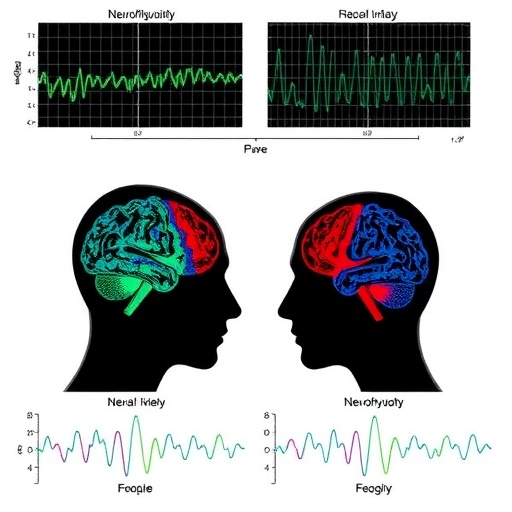
The study hinges on the intricate interplay between brain activity patterns and the therapeutic trajectory of patients experiencing suicidal ideation. Suicidal ideation, often a precursor to suicide attempts, demands timely and effective intervention, yet clinical responses vary dramatically among patients. This heterogeneity calls for objective measures beyond subjective psychiatric evaluations. Neurophysiological biomarkers—measurable indicators derived from brain function—offer a promising pathway. The reviewed evidence points to how changes in electrophysiological signals, such as those captured by electroencephalography (EEG), magnetoencephalography (MEG), and event-related potentials (ERPs), can serve as predictive tools for gauging how patients respond to various treatments, including pharmacotherapy and psychotherapy.
One of the pivotal aspects highlighted in the review is the role of EEG-based biomarkers. EEG measures electrical activity generated by cortical neurons, providing time-sensitive readouts of brain function. Specific EEG components, particularly frontal alpha asymmetry and theta/beta oscillation ratios, emerge as potent indicators linked to emotional regulation and cognitive control mechanisms. Variations in these signals often correlate with differential treatment efficacy, enabling clinicians to potentially tailor interventions based on an individual’s neurophysiological profile. This personalization of treatment aligns strikingly with the broader movement toward precision psychiatry.
Another focal point of the review is the utilization of ERPs—brain responses that are directly the result of a specific sensory, cognitive, or motor event. ERPs have garnered attention due to their sensitivity in detecting cognitive processes affected in suicidal individuals, such as error monitoring and executive function. The systematic evaluation of ERP components like the P300 and N200 waves offers a novel perspective on how brain regions implicated in decision-making and emotional processing respond to therapeutics. Such data underscore the biomarker’s ability to detect subtle yet clinically significant changes during treatment courses.
Importantly, the review does not merely catalogue biomarkers but also critically assesses methodological heterogeneity and limitations within current studies. Variability in sample sizes, treatment modalities, and neurophysiological assessment techniques poses significant challenges to establishing universally accepted biomarkers. However, the authors advocate for refined study designs incorporating longitudinal assessments and multimodal imaging to enhance reliability and validity. They underscore that future research must prioritize replication and consistency to translate these promising findings into everyday clinical tools.
The biological underpinnings tying these neurophysiological markers with suicidal ideation are complex and multifaceted. Dysregulation within fronto-limbic circuits—a network encompassing the prefrontal cortex and limbic regions responsible for emotion regulation—often manifests in aberrant electrophysiological patterns documented in the review. This deregulation may underpin impaired stress response and maladaptive cognitive appraisals, hallmarks of suicidal ideation. Tracking the normalization or aggravation of these patterns during treatment offers a window into the biological effectiveness of interventions, potentially preempting clinical deterioration.
Technological progress grants deeper resolution into these neural signatures. Advanced signal processing methods, machine learning algorithms, and data integration techniques enable researchers to dissect nuanced patterns within high-dimensional neurophysiological data. The review highlights pioneering studies employing artificial intelligence to stratify patients based on biomarker profiles, forecasting who may benefit most from specific therapeutic regimens. These computational innovations promise a future where neurophysiological data can be rapidly interpreted, ushering in real-time biomarker-driven decision-making in psychiatric care.
Furthermore, the review injects critical ethical considerations pertinent to biomarker use in mental health. The prospect of neurophysiological markers predicting suicide risk or treatment response raises pivotal questions about privacy, consent, and the potential stigmatization of individuals based on biomarker status. The authors insist on integrating ethical frameworks during biomarker development and deployment to safeguard patient autonomy and equitable access to care. Such ethical foresight is crucial in navigating the translational pathway from bench to bedside.
Clinical implications extend beyond prediction. Neurophysiological biomarkers may also inform novel therapies such as neuromodulation. Techniques like transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), which modulate neural activity non-invasively, could be optimized by biomarker feedback loops. Tailoring stimulation parameters based on dynamic brain signals and observing biomarker shifts could refine therapeutic precision, maximizing benefits while minimizing side effects. This synergy underscores the biomarker’s potential role in both diagnostics and therapeutics.
The review also discusses the challenge of heterogeneity within suicidal ideation itself. Not all suicidal thoughts share the same intensity, phenomenology, or neurobiological roots. The authors advocate for more granular phenotyping, integrating neurophysiological data with clinical, genetic, and environmental factors. Such integrative models are anticipated to unravel distinct suicidality subtypes, each necessitating unique therapeutic strategies. The systematic review thereby sets a foundation for a multidimensional framework essential for future research and clinical intervention.
It is clear from the evidence synthesized that neurophysiological biomarkers are not a panacea but rather crucial elements in a multifactorial approach to suicide prevention. Their integration with psychological evaluation, behavioral metrics, and biochemical markers forms a comprehensive risk assessment system. The review’s exhaustive analysis propels this multidisciplinary paradigm, emphasizing that the future of suicide intervention hinges on converging empirical evidence from diverse yet complementary domains.
In conclusion, this systematic review published in Translational Psychiatry represents a groundbreaking advance in our understanding of the neurophysiological substrates that underlie treatment response in suicidal ideation. By consolidating existing research and charting pathways for future inquiry, it invites the scientific community to embrace precision neuroscience as a means to more effective, individualized mental health care. As this field matures, these biomarkers hold promise to transform clinical practice from reactive symptom management to proactive, biomarker-informed intervention, potentially saving thousands of lives worldwide.
The journey ahead is one of rigorous validation, ethical vigilance, and technological innovation. How soon these neurophysiological insights will seamlessly integrate into the clinic remains to be seen, but the momentum is undeniable. The stakes could not be higher, as timely identification and intervention for suicidal ideation remain one of psychiatry’s greatest imperatives. This review is a clarion call—neuroscience is poised to redefine suicide prevention for a new generation.
Subject of Research: Neurophysiological biomarkers predicting treatment response in individuals with suicidal ideation.
Article Title: Neurophysiological biomarkers of treatment response in suicidal ideation: a systematic review.
Article References:
Stapper, N., Benster, L.L., Menon, S. et al. Neurophysiological biomarkers of treatment response in suicidal ideation: a systematic review. Transl Psychiatry 15, 473 (2025). https://doi.org/10.1038/s41398-025-03477-2
Image Credits: AI Generated
DOI: 17 November 2025