In the realm of pediatric oncology, retinoblastoma stands as the most prevalent intraocular malignancy among children, posing significant challenges despite advances in treatment modalities. While current therapeutic approaches have notably improved survival rates, the persistent issues of treatment toxicity, tumor relapse, and resistance underscore a pressing need for deeper insights into the molecular and cellular landscape of this tumor. A recent groundbreaking study employing spatial transcriptomics has illuminated the complex heterogeneity within retinoblastoma tumors, offering a novel lens through which to understand intra-patient variability at an unprecedented resolution.
Retinoblastoma tumors are characterized histologically by a spectrum of differentiation states, ranging from poorly differentiated, highly proliferative cells to well-differentiated areas resembling mature retinal cells. This morphological diversity complicates both diagnosis and treatment, with the benign, non-proliferative retinocytoma often presenting diagnostic ambiguities when compared to well-differentiated retinoblastoma subtypes. Previous multi-omics and single-cell transcriptomics analyses have underscored the heterogeneity within retinoblastoma, revealing distinct molecular subtypes that correlate with patient outcomes. Nonetheless, a direct spatial mapping of these diverse cellular populations within the tumor microenvironment had remained elusive—until now.
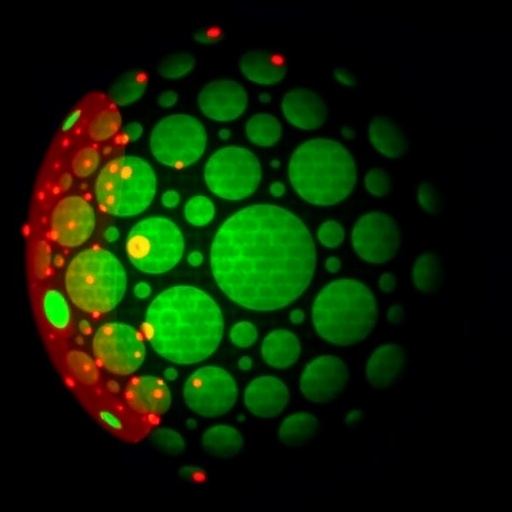
The study in question harnessed the power of spatial transcriptomics to dissect a primary enucleated retinoblastoma specimen exhibiting two distinct histopathological regions. By analyzing sixteen regions of interest that spanned areas of varying differentiation as well as adjacent non-tumoral retinal tissue, researchers were able to integrate transcriptomic data with spatial localization, thereby correlating molecular signatures to specific tumor niches. This high-resolution approach enabled the detection of unique gene expression patterns tied to differentiation status within the same tumor mass, providing compelling evidence of intratumoral heterogeneity visualized directly in situ.
Through unsupervised clustering analyses of transcriptomic profiles, the regions segregated into two main clusters that mirrored histological findings: one cluster encompassed highly differentiated tumor areas enriched in phototransduction-related gene expression, while the other contained poorly differentiated, proliferative regions. Immunohistochemical validation of identified markers in these pathways fortified the transcriptomic data, cementing the link between molecular characteristics and morphological features. This colocalization offers an unprecedented window into how diverse cellular states coexist and potentially drive tumor behavior within individual retinoblastoma cases.
Building on these findings, the study mapped the regions of interest to previously established retinoblastoma molecular subtypes. Subtype 1, characterized by less aggressive behavior and fewer genetic alterations, perfectly aligned with well-differentiated tumor clusters, whereas subtype 2, associated with higher malignancy and metastatic potential, corresponded with poorly differentiated regions. This precise spatial delineation of molecular subtypes within a single tumor mass marks a significant advance in understanding tumor biology and heterogeneity, and it may pave the way for more tailored therapeutic strategies.
A particularly intriguing aspect of this work pertains to the diagnostic challenge surrounding retinocytoma. Despite histological resemblance between retinocytoma and the well-differentiated subtype 1 retinoblastoma areas identified, transcriptomic analysis of senescence-related markers failed to support a retinocytoma diagnosis in the sampled tissue. This suggests that some tumors previously classified based on morphological criteria alone may, in fact, represent distinct subtypes of retinoblastoma with overlapping features. The implications for clinical practice are profound, emphasizing the urgent need for more specific biomarkers to accurately distinguish these entities and guide treatment decisions.
The application of spatial transcriptomics in this context not only enriches the molecular taxonomy of retinoblastoma but also provides an invaluable spatial framework that situates gene expression profiles within their histological context. Such an integrative approach exemplifies the evolving paradigm in cancer research, where single-cell and spatially resolved omics converge to elucidate tumor architecture and its functional consequences. This technological convergence is crucial for unraveling the complexities of intratumoral heterogeneity that directly impact therapeutic resistance and disease progression.
Importantly, the study underscores how spatial heterogeneity within a single tumor can harbor regions with divergent biological behaviors and potential metastatic risks. Recognizing these differences is essential for clinicians seeking to devise more nuanced treatment regimens that can effectively target aggressive tumor subpopulations without overtreatment of less malignant areas. By capturing this mosaicism at spatial and molecular levels, spatial transcriptomics sets the stage for precision oncology in retinoblastoma.
This pioneering research also highlights a broader challenge in pediatric oncology: the fine line between benign and malignant phenotypes when tumors present overlapping histological traits. The inability to conclusively identify senescence markers characteristic of retinocytoma in the well-differentiated tumor areas suggests that reliance on histology alone may be insufficient for accurate diagnosis. The future of diagnosis in retinoblastoma likely lies in adopting multiplexed molecular assays that integrate spatial information, thus enhancing diagnostic accuracy and enabling the stratification of patients for optimal therapies.
Moreover, the methodology showcased by this study exemplifies how spatial transcriptomics can be effectively applied to archived pathological specimens, broadening the scope of retrospective analyses and facilitating the discovery of novel biomarkers. This approach holds promise not only in retinoblastoma but also across various solid tumors where intratumoral heterogeneity complicates clinical management.
The insights garnered here pave the way for future research directions, including the identification of specific gene signatures or cellular markers unique to the different retinoblastoma subtypes and differentiation states. Advancing these molecular signatures could improve prognostication, surveillance for recurrence, and perhaps even uncover new therapeutic targets designed to tackle resistant tumor clones embedded within heterogeneous masses.
Furthermore, integrating spatial transcriptomics with additional omics modalities—such as proteomics and epigenomics—could offer multidimensional portraits of tumor biology, shedding light on regulatory mechanisms that govern differentiation, proliferation, and immune evasion in retinoblastoma. Such integrative studies will be critical for constructing comprehensive tumor atlases that reflect cellular diversity and its clinical ramifications.
The study also serves as a conceptual benchmark for how investigating intrapatient heterogeneity at spatial and molecular scales is not merely an academic exercise but a practical necessity. By revealing the juxtaposition of molecular subtypes within single tumors, this research cautions against one-size-fits-all therapeutic tactics and advocates for adaptive treatment frameworks that can accommodate tumor complexity.
Ultimately, these findings posit spatial transcriptomics as a transformative platform that bridges the divide between histopathology and molecular oncology. By furnishing a visual and genomic map of retinoblastoma tumors, this approach enriches our grasp of tumor biology and accelerates the transition from descriptive pathology to actionable molecular medicine in childhood eye cancers.
As retinoblastoma research advances, continued emphasis on spatially resolved molecular techniques will be pivotal in decoding tumor ecosystems. Bridging these insights with translational efforts promises to yield more precise diagnostic tools and personalized therapies that can mitigate the burden of this devastating pediatric cancer while preserving vision and quality of life.
The convergence of innovative spatial omics technologies with clinical oncology heralds a new era where the intricate microarchitecture of tumors can be charted accurately and therapeutically harnessed. The study’s revelations epitomize this shift, demonstrating that within the apparent uniformity of a tumor lies a heterogenous landscape ripe for exploration and targeted intervention.
In conclusion, the integration of spatial transcriptomics into retinoblastoma research not only demystifies intratumoral heterogeneity but also surfaces critical diagnostic challenges, setting a foundation for enhanced stratification and treatment paradigms. The quest to distinguish subtle tumor subtypes visually and molecularly will undoubtedly inspire future innovations in pediatric cancer diagnostics and therapeutics.
Subject of Research: Retinoblastoma intratumoral heterogeneity characterized through spatial transcriptomics.
Article Title: Spatial transcriptomics of retinoblastoma: a visual window on intra-patient heterogeneity.
Article References:
Moulin, A.P., Thevenet, J., Mazzeo, L. et al. Spatial transcriptomics of retinoblastoma: a visual window on intra-patient heterogeneity. BMC Cancer 25, 1410 (2025). https://doi.org/10.1186/s12885-025-14814-5
Image Credits: Scienmag.com