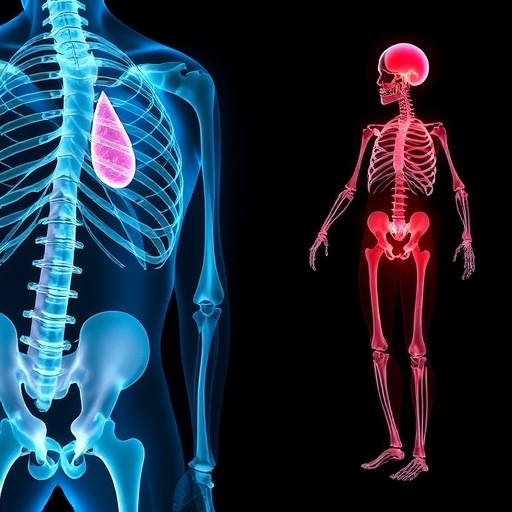
In a significant advancement in understanding the intersection between metabolic disorders and skeletal health, researchers have identified a novel association between high mobility group box 1 (HMGB1) protein and Toll-like receptor 4 (TLR4) as potential biomarkers for assessing osteoporosis risk in individuals diagnosed with type 2 diabetes mellitus (T2DM). This groundbreaking study, conducted by Zhu et al., presents a detailed cross-sectional analysis focusing on how these molecular indicators may illuminate the underlying mechanisms linking diabetes and bone quality deterioration, which has far-reaching implications for clinical practices and patient care.
The study drew on a sizable population sample comprising individuals with T2DM, meticulously measuring serum levels of HMGB1 and the expression of TLR4. Researchers hypothesized that the chronic inflammatory state characteristic of T2DM could lead to dysregulated bone remodeling processes, thereby increasing the likelihood of osteoporosis and related fractures. By investigating the relationships among these biomarkers, the researchers aimed to provide insights into the biological pathways that contribute to increased fragility in diabetic patients’ skeletal systems.
Potentially pivotal in the research was the analysis of HMGB1, a nuclear protein implicated in various cellular processes, including gene expression and inflammation. Elevated levels of this protein have been associated with adverse outcomes in a range of conditions, including autoimmune diseases and cancer. In the context of T2DM, HMGB1 may serve as a pathogenic mediator, enhancing inflammatory responses that ultimately affect osteoblast and osteoclast function. The study underscored the protein’s role in modulating the pathways connected to bone metabolism, thus positioning HMGB1 as a key player in diabetic osteoporosis.
Moreover, the investigation into TLR4 further solidified the findings. This receptor is essential in the innate immune response, recognizing pathogens and orchestrating inflammatory signaling cascades. In T2DM, heightened TLR4 activation has been linked with exacerbated inflammation, which could lead to osteopenic conditions through disrupted bone homeostasis. The correlation between TLR4 expression and osteoporosis risk suggests that targeting inflammatory pathways may be a viable strategy to mitigate bone loss in diabetic populations.
Researchers employed a range of sophisticated statistical analyses to ensure robustness in their findings. The cross-sectional study design not only provided a snapshot of the associations between HMGB1, TLR4, and osteoporosis risk but also allowed for the identification of confounding factors that could impact the observed relationships. Adjustments for age, sex, duration of diabetes, and other metabolic parameters were critical to ascertain the independent contributions of HMGB1 and TLR4 to bone health outcomes.
Significantly, the findings of Zhu et al. revealed that elevated levels of HMGB1 were closely associated with increased TLR4 expression in patients, which in turn correlated with lower bone mineral density (BMD) values and higher osteoporosis prevalence. This pattern illuminated the potential for both HMGB1 and TLR4 to serve not only as biomarkers but also as targets for therapeutic intervention. The concept of using anti-inflammatory strategies to attenuate bone loss could revolutionize the management of osteoporosis in individuals with T2DM.
The implications of this research extend beyond academic curiosity; they may lead to transformative changes in how osteoporosis risk is assessed and managed in diabetic populations. Modern medicine increasingly acknowledges the interconnectedness of bodily systems, and the study reinforces the need for an integrated approach to patient health that considers both metabolic and skeletal aspects. Practitioners and clinicians may need to incorporate routine assessments of HMGB1 and TLR4 levels in diabetic patients, ensuring that those at risk for osteoporosis receive timely and appropriate interventions.
Moreover, the research raises pivotal questions for future studies. If HMGB1 and TLR4 are confirmed as reliable biomarkers, what therapeutic strategies could potentially modulate their levels? This inquiry could pave the way for the development of novel pharmacological agents focused on these targets, offering hope for improved patient outcomes. Additionally, the exploration of lifestyle modifications that may influence HMGB1 and TLR4 levels offers an exciting avenue for both preventative and therapeutic strategies.
Critically, further longitudinal studies will be necessary to validate these findings. While the cross-sectional nature of the current research provides compelling insights, a longitudinal approach would better detail how fluctuations in HMGB1 and TLR4 impact bone density over time in diabetic patients. Understanding these dynamics could lead to more refined risk stratification protocols and personalized treatment plans.
As this research continues to gain visibility within both the scientific community and the public domain, it highlights an urgent need for increased awareness regarding the fragility experienced by those living with diabetes. The common misconception that diabetes solely affects metabolic health must be challenged, emphasizing that it extends to bone health and overall well-being. Educating both patients and healthcare providers on the risks of osteoporosis associated with T2DM could lead to earlier detection and more proactive management approaches.
In conclusion, the identification of HMGB1 and TLR4 as biomarkers for osteoporosis risk in patients with type 2 diabetes mellitus opens a new frontier in metabolic research and clinical practice. As scientists work to unravel the complex interplay between these molecules and the skeletal system, there is an urgent call for innovation in treatments and preventive measures. The hope is that this crucial research spur interdisciplinary collaborations that bring together endocrinologists, orthopedists, and researchers to foster a comprehensive strategy against the silent epidemic of osteoporosis in individuals suffering from diabetes.
The journey of understanding and combating osteoporosis in the context of type 2 diabetes has only just begun, but with studies like this one setting the precedent, there is optimism that we can illuminate effective pathways forward. As research evolves, the integration of biochemical insights and clinical application promises a future with improved outcomes for millions affected by both conditions.
Subject of Research: Biomarkers for osteoporosis risk in type 2 diabetes mellitus.
Article Title: HMGB1 and TLR4 as biomarkers for osteoporosis risk in type 2 diabetes mellitus: a cross-sectional study.
Article References: Zhu, G., Kan, C., Cao, C. et al. HMGB1 and TLR4 as biomarkers for osteoporosis risk in type 2 diabetes mellitus: a cross-sectional study. BMC Endocr Disord 25, 175 (2025). https://doi.org/10.1186/s12902-025-01998-x
Image Credits: AI Generated
DOI: 10.1186/s12902-025-01998-x
Keywords: HMGB1, TLR4, osteoporosis, type 2 diabetes mellitus, biomarkers, inflammation, bone density.