An international consortium of researchers has unveiled the most extensive global-to-local examination to date of the risk factors associated with long COVID, leveraging disability metrics collected at the pandemic’s peak to pinpoint populations vulnerable to prolonged post-infection symptoms. Using the robust framework provided by the Global Burden of Disease (GBD) 2021 study, the team analyzed years lived with disability (YLDs) attributed to COVID-19 across an unprecedented 920 global locations spanning 2020 and 2021. Their findings highlight YLDs as a potentially valuable early biomarker for long COVID risk, especially in regions where post-COVID conditions tend to be underreported or poorly tracked.
The analysis conducted utilized granular disability data, allowing researchers to move beyond traditional case count metrics and focus on the functional impacts endured by patients. This novel approach is critical because long COVID manifests through a constellation of chronic symptoms that impair quality of life and daily functioning but may be overlooked in acute case surveillance. By quantifying YLDs—an epidemiological measure representing years lived with health complications weighted by severity—the team aimed to capture the hidden burden of lingering COVID sequelae that typical reporting mechanisms fail to address.
Dan Shan, co-first author of the study, emphasized the significance of disability-focused data as an early warning system for emerging long COVID hotspots. “Many communities, particularly those in resource-limited settings, were enduring disproportionately high levels of disability well before long COVID was widely recognized,” Shan noted. The failure to intervene promptly could result in prolonged suffering and elevated healthcare burdens, compounding inequities that already exist due to socioeconomic disparities.
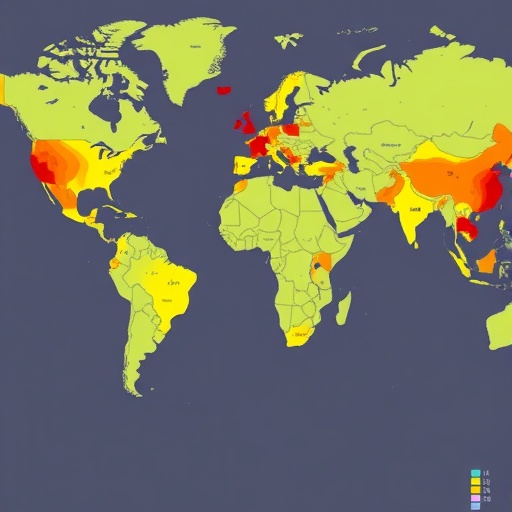
The study revealed stark disparities in the global distribution of long COVID-associated disability. In 2021, eight of the top ten countries exhibiting the highest age-standardized YLD rates were categorized as low-, lower-middle-, or middle-income nations. Countries such as Mozambique, Malawi, Ethiopia, and Iraq exemplified this troubling trend. These regions frequently suffer from under-resourced healthcare systems, which are ill-equipped to detect, report, and manage post-acute COVID-19 conditions. This structural weakness significantly hampers their ability to accurately quantify and tackle the long-term impacts of the pandemic.
Gender-based analysis also surfaced noteworthy patterns. Females aged 20 and above bore a significantly greater burden of YLDs than their male counterparts, corroborating existing epidemiological evidence suggesting sex-based vulnerability in long COVID outcomes. This disparity underscores the importance of integrating sex- and gender-sensitive frameworks into both research methodologies and public health interventions aimed at understanding and mitigating long COVID’s reach.
While wealthier nations generally exhibited lower overall YLD metrics, the research underscored that national averages obscure profound sub-national inequalities. The United States serves as a prime example, where long COVID risk varied notably across states and communities. Rural areas and underserved populations bore a disproportionate share of the YLD burden, reflecting systemic healthcare access disparities, socioeconomic deprivation, and potential environmental factors compounding health outcomes. Such heterogeneity within affluent countries suggests that macro-level epidemiological data are insufficient for directing focused long COVID remediation efforts.
Shan highlighted, “Even within high-income countries, the distribution of long COVID’s effects is uneven, with specific communities facing far worse outcomes. Policy responses must therefore prioritize granularity to identify and assist these vulnerable pockets, lest they remain invisible in population-level statistics.” This insight calls for enhanced data collection practices that disaggregate information by geography, socioeconomic status, race, and other social determinants of health.
Central to the researchers’ conclusions is an urgent call for expanding long COVID care infrastructure globally, with prioritization accorded to low-resource settings that bear the heaviest burdens but have the least capacity for intervention. They advocate for the integration of standardized disability metrics into early warning systems for pandemic response and long COVID surveillance. Such data integration would create actionable intelligence, enabling healthcare providers and policymakers to anticipate and allocate resources effectively.
Moreover, the study highlights the need for international health agencies to recalibrate funding priorities, emphasizing rehabilitation services that address complex, multi-system long COVID syndromes in vulnerable groups. Research investment must similarly pivot to unraveling the pathophysiological mechanisms driving differential risk profiles geographically and demographically, to inform targeted therapeutic approaches. Building surveillance infrastructure capable of tracking disability trends longitudinally is critical not only to monitor current impacts but also to brace for future post-infectious sequelae of viral pandemics.
The global community faces a crossroads: ignore these emerging signals of long-term disability and risk exacerbating health inequities, or mobilize a coordinated, data-driven response that foregrounds equity, precision, and compassion. The findings underscore that the consequences of COVID-19 extend well beyond acute illness, embedding themselves into the fabric of public health through chronic morbidity that demands sustained attention.
By leveraging sophisticated epidemiological methodologies and unprecedented global datasets, this study reframes long COVID risk from a vague, anecdotal concern to a tangible, quantifiable public health crisis. It challenges existing paradigms of pandemic recovery, advocating a shift toward chronic disease management frameworks and reinforcing the importance of health system resilience in safeguarding communities worldwide.
In summary, the research not only charts the geographic and demographic contours of early pandemic-related disability but also establishes disability data as a cornerstone for anticipating long COVID’s trajectory. It propels the conversation forward, urging global health actors to embrace comprehensive, equity-focused strategies that mitigate disparities and foster recovery for all affected populations.
Subject of Research: Assessment of long COVID risk through global and local disability data using years lived with disability (YLDs) metrics from the Global Burden of Disease 2021 framework.
Article Title: (Not specified in the content)
Web References: http://dx.doi.org/10.1002/mdr2.70023
Image Credits: Dan Shan
Keywords: Public health, long COVID, COVID-19, disability data, Global Burden of Disease, epidemiology, health disparities, chronic illness, rehabilitation, health equity