Researchers unveil a groundbreaking immune-based genomic signature that promises to revolutionize treatment strategies for hormone receptor-positive, HER2-negative breast cancer by predicting patient responses to CDK4/6 inhibitors, a cornerstone therapy for this cancer subtype. This advancement, emerging from a collaborative study led by IrsiCaixa, the Catalan Institute of Oncology (ICO), and the Germans Trias i Pujol Research Institute, represents a crucial leap toward personalized oncology and improved clinical outcomes.
Cyclin-dependent kinase 4 and 6 (CDK4/6) inhibitors, combined with hormone therapy, have transformed the therapeutic landscape for advanced HR+/HER2- breast cancer by targeting cell cycle regulatory proteins integral to tumor proliferation. These inhibitors act by halting the cell cycle’s progression from the G1 to the S phase, effectively restraining cancer cell division and tumor growth. Despite the efficacy of this dual treatment approach, resistance and variable patient responses remain significant clinical challenges, underscoring the urgent need for predictive biomarkers.
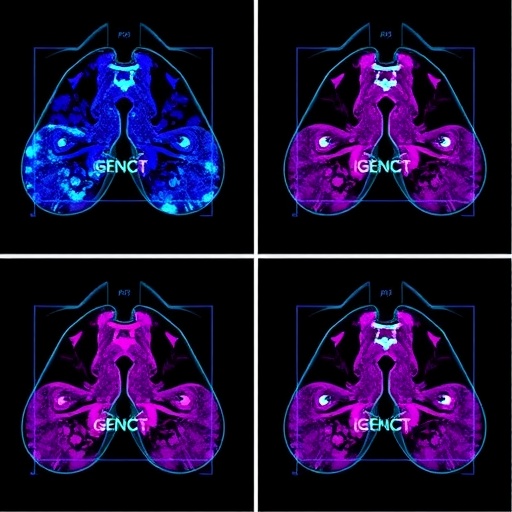
In a meticulous study involving almost one hundred patients treated at ICO Badalona under the CARE programme, the research team identified a distinctive transcriptomic signature named KIMA (Key Immune Activation). KIMA enables oncologists to forecast a patient’s likelihood of poor response to CDK4/6 inhibitors based on the expression profile of specific immune-related genes. This discovery not only holds potential for predicting therapeutic efficacy but also opens novel avenues for combinatorial treatments incorporating immunomodulation.
The clinical cohort revealed striking differences in treatment outcomes, with 57% of patients achieving durable responses exceeding two years without tumor progression, while 43% experienced early relapse within months. Detailed transcriptomic analyses demonstrated that those patients with adverse outcomes harbored tumors exhibiting aberrant immune activation. This immune signature paradoxically correlates with an immunosuppressive tumor microenvironment, facilitating therapeutic resistance rather than promoting tumor eradication.
KIMA is composed of nine genes, including pivotal immune regulators such as STAT1, FOXP3, and TIGIT. The collective overexpression of these genes in the tumor milieu predicts a significantly diminished prognosis, characterized by accelerated disease progression and poor overall survival. Quantitatively, patients with elevated KIMA expression exhibited a median progression-free survival of approximately 11 months, starkly contrasted with about 36 months in those with low KIMA levels, highlighting its robust prognostic value.
The validity of KIMA was further corroborated through an independent clinical study, which confirmed that non-responders to CDK4/6 inhibitors possess distinct, high-level expression profiles of this immune activation signature. This consistency across datasets underpins KIMA’s potential utility as a clinical decision-making tool, facilitating earlier intervention strategies tailored to the molecular intricacies of each patient’s tumor.
Intriguingly, the study challenges the conventional paradigm that immune activation equates to effective anti-tumor immunity. Instead, in HR+/HER2- breast cancer, hyperactivation of certain immune pathways appears to foster a tumor-supportive environment, possibly through immune checkpoint pathways and regulatory T cell-mediated suppression. This insight sheds light on the complex interplay between tumor biology and the immune system’s dualistic role in cancer progression and therapeutic resistance.
The authors highlight the translational impact of this research, suggesting that patients identified with a high KIMA signature might benefit from novel therapeutic combinations. These could include the addition of innovative immunomodulatory agents aiming to reprogram the tumor microenvironment, thereby restoring immune surveillance and enhancing CDK4/6 inhibitor efficacy. Such personalized approaches promise to optimize treatment regimens and improve patient survival.
Leading the investigation, Dr. Eudald Felip and Dr. Edurne Garcia-Vidal emphasize the importance of integrating immune profiling into routine clinical practice for HR+/HER2- breast cancer. The identification of non-responders through genomic signatures like KIMA could prevent ineffective treatments and unnecessary toxicity while sparing healthcare resources, marking a significant stride in precision oncology.
The research consortium, including Dr. Ester Ballana and Dr. Mireia Margelí, underscores that harnessing the immune system’s intricacies and understanding its regulatory networks within cancerous tissues is pivotal for future therapeutic innovations. This study exemplifies the synergy between molecular biology, oncology, and immunology, providing a template for investigating resistance mechanisms in other cancer types.
Moving forward, large-scale clinical trials incorporating KIMA stratification are planned to validate its predictive power further and assess the efficacy of combined CDK4/6 inhibitor and immunotherapy protocols. Such efforts will be crucial in translating this signature from bench to bedside, ultimately improving survival and quality of life for patients battling HR+/HER2- breast cancer.
The discovery of KIMA and its clinical implications heralds a new chapter in breast cancer treatment, emphasizing the necessity to delve deeper into tumor immunogenomics. Through understanding and overcoming therapeutic resistance, this landmark study brings hope that the era of truly personalized medicine for breast cancer patients is imminent.
Subject of Research: Cells
Article Title: Immune-based transcriptomic signature predicts CDK4/6 inhibitor efficacy in HR+/HER2– breast cancer
News Publication Date: 7-Aug-2025
Web References: http://dx.doi.org/10.1002/ctm2.70426
Image Credits: ICO-IrsiCaixa-IGTP
Keywords: Breast cancer, Cancer, Oncology, Biomarkers, Immunology