In an era where mental health challenges are increasingly recognized as critical global health concerns, a groundbreaking study published in BMC Psychiatry introduces new insights into the complex interplay between demoralization and resilience traits. This research delves into the psychological mechanisms underpinning demoralization—a debilitating mental state marked by a profound loss of purpose, hopelessness, feelings of worthlessness, and even suicidal ideation. Utilizing sophisticated network analysis techniques, the study unpacks how demoralization interacts with established trait resilience factors such as locus of control and general self-efficacy.
Demoralization, though often conflated with depression and anxiety, embodies a distinct construct characterized primarily by poor coping abilities and existential despair. To quantify this, the researchers employed the revised Demoralization Scale (DS-II), specifically the Münster version (DS-II-Ms), allowing for precise measurement and comparative analysis within the general population. Prior investigations had validated the DS-II-Ms’s psychometric properties and its correlations with depression and anxiety, laying a robust foundation for this deeper exploration into resilience links.
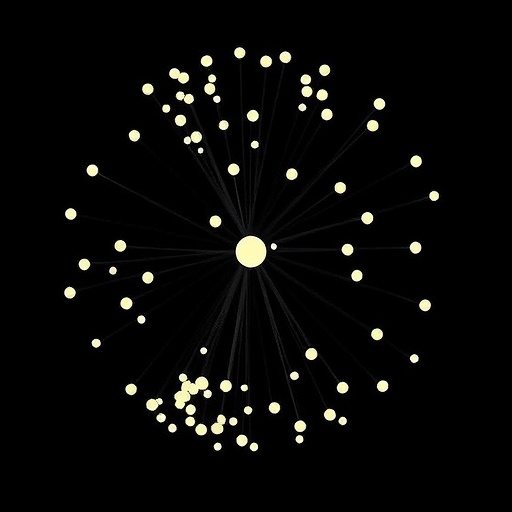
The team administered a battery of validated psychological instruments, including DS-II-Ms, the Patient Health Questionnaire-2 (PHQ-2), the Generalized Anxiety Disorder Scale-2 (GAD-2), the Internal-External Locus of Control Short Scale-4 (IE4), the General Self-Efficacy Short Scale-3 (GSE-3), and the Brief Resilience Scale (BRS) to a representative sample of 2,401 German adults. This comprehensive dataset permitted the construction of a Gaussian graphical model, a statistical framework adept at revealing unique, conditional relationships among variables after accounting for shared variance, thereby illuminating the nuanced structure connecting demoralization and resilience traits.
The network analysis results revealed a moderate association between demoralization and locus of control, notably, individuals exhibiting higher demoralization tended to report a lower internal locus of control and a higher external locus of control. This suggests a diminished perception of personal agency and increased attribution of outcomes to external forces among demoralized individuals. Interestingly, demoralization appeared conditionally independent of the Brief Resilience Scale and general self-efficacy, marking a potential divergence in the resilience dimensions that relate to demoralization versus other psychological conditions.
Conversely, symptoms of depression, particularly those involving lack of interest and low mood, formed connections with resilience and general self-efficacy domains, but crucially, these symptoms were conditionally independent of locus of control measures. This dichotomy underscores that while related, demoralization and depression engage different aspects of psychological resilience, reinforcing the conceptual distinctions between these constructs and their underlying mechanisms.
The implications of these findings are profound for therapeutic interventions targeting mental health disorders. By demonstrating that trait resilience factors uniquely associate with demoralization and depression/anxiety symptoms respectively, the study challenges the one-size-fits-all approach in mental health treatment paradigms. Specifically, it advocates for the development of tailored interventions that address precise resilience constructs pertinent to a patient’s symptom profile, potentially enhancing treatment efficacy and patient outcomes.
Despite the illuminating insights, the authors acknowledge the inherent limitations of their cross-sectional study design, which precludes definitive conclusions about causality or directional influence among the examined variables. Longitudinal research is necessary to elucidate the temporal dynamics and causal pathways linking demoralization, resilience traits, and related psychopathologies. Nonetheless, this study provides a crucial stepping stone by mapping the contemporaneous interplay of these factors within a broad population sample.
Moreover, the differentiation of demoralization from depression and anxiety symptoms brings clarity to mental health diagnostic frameworks, which have historically grappled with overlapping symptoms and blurred boundaries between constructs. Identifying demoralization as a separate clinical entity has significant ramifications for both research and clinical practice, emphasizing the need for specialized screening tools and targeted psychotherapeutic strategies.
The use of a network psychometrics approach represents a methodological innovation in psychiatry research, allowing for the discernment of complex, conditional dependencies within psychological constructs beyond traditional correlation analyses. This statistical approach aligns well with contemporary models of mental disorders as networks of interacting symptoms and traits rather than as monolithic syndromes, offering a more granular understanding of mental health phenomena.
Furthermore, the reliance on a representative sample of the German general population enhances the external validity of the findings, ensuring that conclusions are not confined to clinical or convenience samples but rather reflect the broad spectrum of mental health and resilience characteristics in the community. This broad applicability advocates for the integration of these findings into public health strategies aimed at bolstering psychological resilience and mitigating demoralization at a population level.
As the field moves forward, the nuanced understanding provided by this study paves the way for interdisciplinary collaborations combining clinical psychology, psychiatry, psychometrics, and public health. These efforts could unravel the biological, psychological, and social underpinnings of resilience and demoralization, fostering comprehensive, personalized care paradigms that accommodate the diversity of human psychological experiences.
This study’s revelations hold promise not only for advancing theoretical knowledge but also for practical applications in mental health interventions, policy development, and resilience training programs. By pinpointing specific resilience factors that are distinctively linked to demoralization, mental health professionals can fine-tune their therapeutic approaches, potentially reducing the incidence and impact of demoralization and its tragic sequelae, such as suicidal ideation.
In summary, the pioneering work published by Ramm et al. in BMC Psychiatry illuminates a critical aspect of mental health that has hitherto been underexplored—the differential relationship between demoralization and trait resilience factors within the general population. Employing robust psychometric instruments and state-of-the-art analytical methods, this research unearths distinct pathways through which demoralization interacts with locus of control, while highlighting its divergence from general self-efficacy and broader resilience measures. These insights not only advance psychiatric research but also lay a conceptual and empirical foundation for more focused and effective clinical interventions in mental health.
Subject of Research: The relationship between demoralization and trait resilience factors including locus of control and general self-efficacy, using network psychometrics in a representative population sample.
Article Title: How demoralization is related to trait resilience factors: a network analysis in a representative sample of the general population
Article References:
Ramm, M., Schnabel, K., Jedamzik, J. et al. How demoralization is related to trait resilience factors: a network analysis in a representative sample of the general population. BMC Psychiatry 25, 975 (2025). https://doi.org/10.1186/s12888-025-07487-8
Image Credits: AI Generated