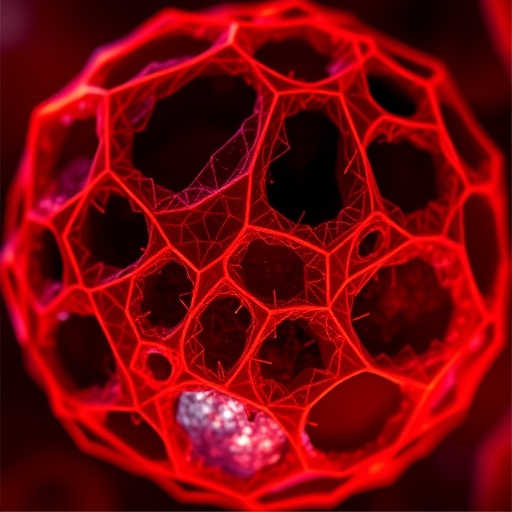
Recent groundbreaking research published in the prestigious journal Cell reveals a fascinating and previously uncharted feature on the surface of melanoma cells: immune “craters.” These crater-like structures serve as specialized hubs that significantly enhance the engagement between tumor cells and CD8+ T cells, a critical component of the immune system’s arsenal against cancer. This discovery not only deepens our understanding of the tumor microenvironment but also offers promising new markers for evaluating the success of immunotherapy, potentially revolutionizing cancer treatment strategies.
Immune checkpoint blockade (ICB) therapy represents a paradigm shift in oncology by reactivating the patient’s own immune cells, particularly CD8+ cytotoxic T lymphocytes, to attack and eradicate tumor cells. However, the precise mechanisms that underpin localized tumor targeting and effective killing have remained enigmatic. Addressing this gap, the new study employed advanced live imaging within a uniquely conducive zebrafish melanoma model, enabling researchers to observe CD8+ T cell behavior in an intact tumor over an extensive 24-hour period. Zebrafish offer unparalleled capabilities for continuous live tracking due to their transparency and biocompatibility, allowing scientists to visualize complex cell interactions in real time.
The research team, led by Dr. Leonard Zon of Boston Children’s Hospital, identified that CD8+ T cells do not distribute evenly across the tumor landscape. Instead, these immune cells cluster within discrete pockets at the melanoma periphery that the investigators termed “Cancer Regions of Antigen presentation and T cell Engagement and Retention,” abbreviated as CRATERs. Within CRATERs, T cells formed stable, prolonged contacts with tumor cells, sharply contrasting with the previously held assumption that immune cells continuously patrolled the tumor surface randomly. Upon immune stimulation—mimicking the activation triggered by ICB therapy—CRATER zones were observed to expand, intensifying their immunological activity and enhancing tumor cell destruction.
Strikingly, the existence of CRATERs was not restricted to zebrafish models. Human melanoma samples likewise demonstrated analogous crater formations, reinforcing the translational relevance of these findings in clinical oncology. What’s more, similar immune-tumor interaction sites were detected in human lung cancer tissues, suggesting that CRATERs may be a broader phenomenon occurring across multiple solid tumor types rather than a melanoma-specific anomaly. This cross-tumor consistency hints at a conserved microenvironmental feature that modulates immune response efficacy.
Historically, the clinical assessment of ICB therapy success has relied heavily on indirect metrics such as tumor necrosis, fibrosis, or overall CD8+ T cell infiltration observed in biopsy samples. While these metrics offer some predictive insight, none directly capture the dynamic and intimate cell-cell engagements critical for actual tumor eradication. CRATERs fill this crucial knowledge void by providing a tangible, functional niche where immune cells dock and exert cytotoxic effects. Therefore, CRATER presence and characteristics could emerge as more accurate biomarkers for patient response to immunotherapy than existing surrogate measures.
The discovery of CRATERs also opens new investigative avenues for optimizing ICB therapy. Understanding how these immunological craters form and expand following treatment may enable the design of therapeutic adjuncts that promote or stabilize CRATER formation, thereby boosting the immune system’s tumoricidal capacity. In addition, longitudinal tracking of CRATER dynamics could inform real-time monitoring of treatment efficacy and guide timely therapeutic adjustments for improved patient outcomes.
The study’s implications extend beyond diagnostics and treatment monitoring. It also reshapes fundamental concepts regarding tumor-immune system spatial relationships. The identification of these immune hubs challenges the oversimplified view of homogenous immune cell infiltration and instead reveals a highly organized and compartmentalized immune assault strategy. This insight compels a reevaluation of tumor microenvironment models, demanding integration of three-dimensional architectural and temporal components into immune-oncological research.
With these promising findings, the investigative team is now laying the groundwork for prospective clinical trials aimed at rigorously validating CRATERs as predictive markers in humans undergoing ICB therapy. Such trials will be critical in establishing the sensitivity, specificity, and practical application of CRATER assessment within clinical workflows. Should the clinical data hold true, CRATER-based diagnostics might soon become standard practice, providing oncologists with powerful new tools to personalize cancer immunotherapy.
Mechanistically, the formation of CRATERs involves complex cell-cell communication and antigen presentation processes that effectively “anchor” CD8+ T cells to the tumor surface. This anchorage facilitates prolonged immune synapse formation, enhancing cytolytic granule release and tumor cell apoptosis. Future research is anticipated to dissect the molecular players involved in CRATER formation, including tumor antigens, adhesion molecules, and signaling pathways that orchestrate immune retention and activation within these niches.
The utilization of zebrafish models was pivotal in this discovery, underscoring the value of innovative in vivo imaging techniques in cancer immunology. Conventional murine or human tissue models lack the transparent and accessible properties that zebrafish provide, limiting direct visualization of dynamic immune-tumor interactions over extended durations. This methodological breakthrough exemplifies how model organism selection and technological advances synergize to unlock unseen facets of disease biology.
In summary, the identification of CRATER tumor niches elucidates a critical lynchpin in the immunotherapy success mechanism. By bridging the gap between immune cell infiltration and effective tumor killing, these crater formations represent both a biomarker and a potential therapeutic target. The landscape of cancer immunotherapy stands poised for advancement as further clinical validation and molecular characterization of CRATERs progresses, heralding a new era of precision immuno-oncology.
Subject of Research: Cancer immunotherapy, immune-tumor microenvironment, CD8+ T cell engagement in melanoma and lung cancer
Article Title: CRATER Tumor Niches facilitate CD8+ T cell engagement and correspond with immunotherapy success.
News Publication Date: 17-Oct-2025
Web References:
DOI: 10.1016/j.cell.2025.09.021
Keywords: Cancer immunology, Immunotherapy, Checkpoint therapy, Melanoma, Lung cancer, Zebrafish