In a groundbreaking study published in Medical Oncology, researchers have unveiled the promising therapeutic potential of bone marrow-derived mesenchymal stem cell (BM-MSC) exosomes in modulating the oncogenic long non-coding RNA (lncRNA) TUG1, thereby exhibiting antileukemic effects against THP-1 cells, a human monocytic leukemia cell line. This discovery could herald a significant paradigm shift in leukemia treatment strategies, underscoring the power of extracellular vesicles as biologically active nanocarriers for targeted molecular therapy.
The intricate landscape of leukemia research has long sought innovative approaches to circumvent the limitations of conventional chemotherapy, which often results in systemic toxicity and the emergence of drug resistance. Exosomes, nano-sized vesicles secreted by cells, have surged to the forefront as natural intercellular communication vehicles capable of transferring proteins, lipids, and nucleic acids. These vesicles can modulate recipient cell behavior, and harnessing their innate bioactive cargo offers a refined approach to cancer therapy.
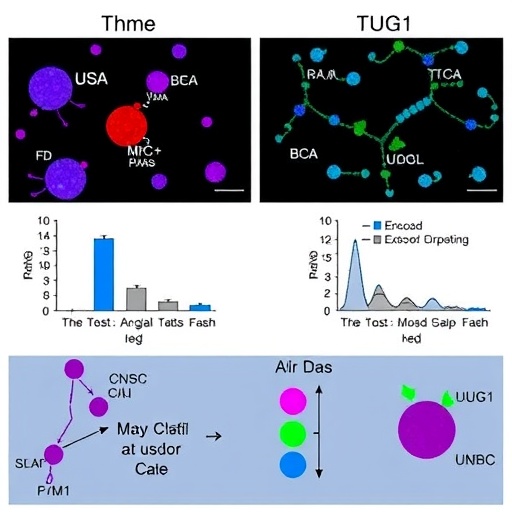
Karimian and colleagues focused their investigation on BM-MSC-derived exosomes due to their inherent immunomodulatory properties and ability to home to tumor microenvironments. The study elucidates how these exosomes deliver regulatory molecules that specifically attenuate the expression of TUG1—a lncRNA implicated in the progression and chemoresistance of acute myeloid leukemia and other malignancies.
TUG1 has emerged as a critical player in oncogenesis, acting through multiple signaling pathways to promote cell proliferation, inhibit apoptosis, and facilitate leukemia cell survival. By targeting TUG1, BM-MSC exosomes initiate a cascade of molecular events that disrupt leukemia cell viability and proliferation. The modulation of TUG1 expression downregulates oncogenic pathways, potentially reversing the malignant phenotype of leukemic cells.
The researchers employed a robust array of molecular biology techniques to validate their findings, including quantitative real-time PCR to assess TUG1 expression levels, cell viability assays, and flow cytometry to determine apoptosis rates in THP-1 cells. The treated cell populations demonstrated significant reductions in TUG1 transcripts alongside marked increases in apoptotic markers, underscoring the exosomes’ efficacy in inducing leukemia cell death.
An intriguing aspect of this study is the demonstration that BM-MSC-derived exosomes can modulate lncRNA expression without genetic modification of the recipient cells. This suggests a non-invasive, biologically harmonious method of gene regulation, circumventing the risks associated with direct nucleic acid therapies such as viral vector delivery or synthetic oligonucleotides, which often face challenges of delivery efficiency and off-target effects.
Moreover, the study highlights the multifunctional nature of exosomes, which carry a diverse molecular cargo. The investigators speculate that components within the exosomes, including microRNAs and specific RNA-binding proteins, may be orchestrating the downregulation of TUG1. Future research will need to dissect the precise molecular constituents responsible for this modulation, offering opportunities for designing engineered exosomes with enhanced therapeutic payloads.
The implications of these findings extend beyond leukemia alone. The lncRNA TUG1 has been implicated in various cancers, suggesting that BM-MSC-derived exosomes could have a broader utility in oncology as modulators of aberrant lncRNAs. This broad-spectrum potential invites optimism for developing exosome-based therapies targeting malignancies with similarly dysregulated non-coding RNAs.
However, clinical translation remains a formidable challenge. The scalability of exosome production, stability in circulation, targeted delivery, and avoidance of immune clearance are critical parameters that must be optimized. Karimian et al.’s work significantly contributes to understanding the mechanistic foundations but also sets the stage for translational research to refine exosome-based therapeutics.
From a mechanistic standpoint, the study delves into how TUG1 influences leukemogenesis through downstream effectors. Evidence suggests TUG1 interacts with chromatin remodeling complexes, modulates miRNA availability, and affects key signaling pathways such as PI3K/AKT and Wnt/β-catenin, all of which contribute to leukemia cell survival and proliferation. By lowering TUG1 levels, BM-MSC exosomes destabilize these pathways.
The therapeutic potential is further reinforced by the observation that exosome treatment did not induce significant cytotoxicity in normal hematopoietic stem cells, indicating a degree of selectivity for malignant cells. This specificity enhances the appeal of exosome-based approaches, potentially reducing collateral damage to healthy tissues often seen in traditional chemotherapy.
Intriguingly, the study opens avenues for combinatorial therapies. BM-MSC exosomes could be integrated with existing chemotherapeutic regimes to potentiate drug sensitivity and overcome resistance mechanisms mediated by lncRNAs. This multipronged approach could improve overall patient outcomes by lowering treatment doses and mitigating side effects.
Furthermore, the immunomodulatory properties of BM-MSC exosomes may contribute to altering the tumor microenvironment, fostering anti-leukemic immune responses. The crosstalk between leukemia cells and their microenvironment underlies disease progression and therapy resistance, thus exosome-mediated interference could disrupt these pathogenic interactions.
The findings bring to light the dynamic role of extracellular vesicles in cancer biology, not merely as biomarkers but as active therapeutic agents capable of fine-tuning complex gene regulatory networks. This elevates our understanding of cell–cell communication in oncogenesis and paves the way to harness the full therapeutic potential of naturally occurring biological nanoparticles.
In conclusion, the study by Karimian and colleagues powerfully demonstrates that BM-MSC-derived exosomes can downregulate the oncogenic lncRNA TUG1 in THP-1 leukemia cells, inducing apoptosis and thwarting malignant progression. This innovative approach offers a novel, biologically inspired modality that could revolutionize leukemia treatment and potentially other malignancies characterized by dysregulated non-coding RNAs. Continued exploration of exosome biology and engineering will be paramount to translating these promising in vitro results into clinical reality, setting a new frontier in precision oncology.
Subject of Research:
The study investigates the role of bone marrow-derived mesenchymal stem cell (BM-MSC) exosomes in modulating the expression of the oncogenic long non-coding RNA TUG1 and their anti-leukemic effects on THP-1 human monocytic leukemia cells.
Article Title:
The potential role of BM-MSC-derived exosomes in TUG1 modulation: antileukemic effects on THP-1 cells.
Article References:
Karimian, F., Loghmani, Z., Vazifeh Shiran, N. et al. The potential role of BM-MSC-derived exosomes in TUG1 modulation: antileukemic effects on THP-1 cells. Med Oncol 42, 544 (2025). https://doi.org/10.1007/s12032-025-03103-7
Image Credits: AI Generated