In a groundbreaking step toward integrating mental health care into chronic illness management, researchers have unveiled a novel audio-based cognitive behavioral therapy (CBT) mobile application specifically designed for patients undergoing hemodialysis. This innovative digital solution emerges from a meticulous development process aimed at addressing the unique psychological challenges faced by these patients, who are particularly vulnerable to depression due to the demanding nature of their treatment regimen. The study, led by Narimanpour, Pirnejad, Makhdoomi, and colleagues, offers promising evidence on the app’s usability, suggesting a potential paradigm shift in how depression can be managed within this population.
Depression is notoriously common among individuals receiving hemodialysis, with prevalence rates significantly higher than in the general population. The psychological burden introduced by chronic kidney disease, compounded by the intensive time commitment and physical toll of dialysis, often results in diminished quality of life and worsened clinical outcomes. Traditional mental health interventions, while effective, face barriers including limited access, stigma, and the physical limitations imposed by treatment schedules. The introduction of a mobile platform leveraging audio-guided CBT techniques represents an adaptive strategy designed to overcome these barriers by offering accessible, scalable, and patient-centric mental health care.
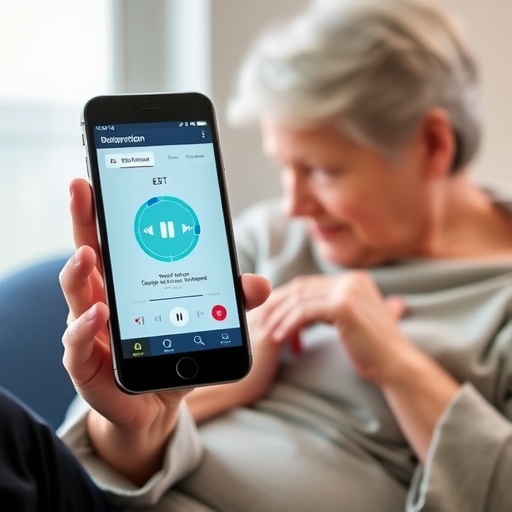
The technical architecture of the app integrates core CBT principles delivered entirely through an audio interface, minimizing the necessity for visual interaction which can be taxing for patients frequently connected to medical devices. This choice of modality is purposeful, recognizing the cognitive and sensory fatigue common in hemodialysis patients. The app’s interface emphasizes simplicity, enabling users to engage with therapy sessions during dialysis or at home without extensive navigation, thereby fostering higher engagement rates and adherence. The developers undertook a user-centered design approach, drawing from extensive qualitative input from patients and clinicians to tailor content and functionality to real-world needs.
The usability evaluation, conducted through a mixed-methods framework, combined quantitative metrics such as task completion rates and error frequencies with qualitative feedback focusing on user satisfaction, perceived effectiveness, and emotional resonance of the therapeutic content. Participants reported that the app’s audio sessions facilitated a calming mindset and provided actionable strategies to manage depressive symptoms. Notably, the on-demand accessibility of the therapy allowed patients to contextualize and apply cognitive restructuring techniques during moments of heightened emotional distress, marking a significant advancement over traditional therapy delivery models that require scheduled sessions.
One of the most compelling features of this innovation lies in its potential to reduce the stigma associated with mental health treatment in somatic illness contexts. By offering a discreet, private platform that patients can utilize independently, the app addresses concerns about social judgment and confidentiality that frequently deter engagement. Furthermore, the audio-based CBT program is structured to empower patients with self-management tools, fostering a sense of autonomy critical to sustained mental health improvement. This aligns with contemporary trends in digital therapeutics, which advocate for patient agency as a cornerstone of effective intervention.
The deployment of this app within dialysis centers also signifies a novel integration of mental health support within somatic care environments. Clinicians involved in the study reported that the app could serve as an adjunct to routine medical treatment, potentially facilitating earlier detection and intervention for depressive symptoms. The researchers envision a future where this technology is embedded in comprehensive care models, augmenting multidisciplinary approaches to chronic kidney disease management. This integration not only promises to enhance patient well-being but may also contribute to improved treatment adherence and overall clinical prognosis.
From a technological standpoint, the backend of the application employs adaptive algorithms to personalize session progression based on user interaction patterns and feedback, promoting relevance and sustained engagement. This dynamic customization is a significant advancement over static digital therapies, which often suffer from high dropout rates due to perceived irrelevance or monotony. The data emerging from this pilot study suggests that patients responded favorably to these tailored pathways, which enhanced the sense of a therapeutic alliance even in the absence of live clinician interaction.
Beyond usability, the researchers conducted preliminary psychometric assessments to explore potential efficacy markers. While the primary aim of the study was to establish feasibility, early indications of mood improvement were observed, correlating with session frequency and consistency of app usage. These findings pave the way for larger clinical trials aimed at rigorously evaluating the therapeutic impact of audio-based mobile CBT in hemodialysis populations. The prospect of a low-cost, scalable digital intervention capable of mitigating depressive symptoms holds substantial implications for public health, especially in resource-limited settings.
The research team also acknowledged the challenges inherent in deploying digital mental health solutions among a medically and demographically heterogeneous group. Variations in age, education level, and technological literacy necessitated the development of comprehensive onboarding processes, including easy-to-follow tutorials and technical support mechanisms. This attentiveness to user diversity underscores the importance of inclusivity in digital health innovation and suggests best practices for future developments targeting similarly complex patient cohorts.
Security and privacy considerations were paramount throughout the app’s design, with stringent encryption protocols safeguarding sensitive user data. Recognizing the sensitive nature of psychological health information, the app’s compliance with healthcare data protection regulations was ensured, and transparent data usage policies were communicated to users. This focus not only supports ethical standards but also builds user trust—an essential component in digital therapeutic success.
Another intriguing aspect of the app is its potential adaptability to other chronic disease populations facing parallel psychological burdens. The modular nature of the audio content facilitates customization for diseases such as diabetes or heart failure, where depression prevalence also adversely impacts outcomes. This adaptability could transform the digital CBT landscape, offering a versatile therapeutic platform with broader applicability beyond its initial scope.
Given the rigorous usability validation and positive patient reception, healthcare providers and policymakers are encouraged to consider the integration of such digital therapeutics into existing mental health infrastructure. The scalability of mobile health solutions could address systemic gaps in psychiatric service accessibility, particularly in rural or underserved areas with limited specialized care. As mobile device penetration continues to surge globally, these audio-based interventions herald a new era where mental health care becomes ubiquitous, patient-friendly, and seamlessly integrated into chronic illness management.
Looking forward, the researchers advocate for iterative refinement based on real-world user data, including enhancements in interactivity and incorporation of biometric feedback to more dynamically respond to patient states. The fusion of machine learning to optimize therapeutic content flow and predictive analytics to identify relapse signals represents an exciting frontier that could further personalize and amplify treatment benefits. This study, therefore, lays foundational groundwork for a future where digital mental health tools not only support but actively augment clinical decision-making and patient self-care.
The convergence of technology, psychology, and nephrology embodied by this audio-based CBT app exemplifies the interdisciplinary innovation necessary to tackle complex health challenges. By harnessing the accessibility of mobile platforms and the evidence-based efficacy of cognitive behavioral therapy, the team has charted a novel path toward holistic, patient-centered care. As the global burden of chronic kidney disease and depression continues to climb, such pioneering solutions are critical to enhancing patient quality of life and mitigating the extensive healthcare costs associated with comorbid mental health disorders.
In conclusion, this study heralds a transformative approach to mental health management in chronic disease settings, offering robust evidence that audio-based mobile CBT is not only feasible and well-received but also holds significant promise for improving depression outcomes in hemodialysis patients. The implications extend far beyond this specific patient cohort, suggesting a scalable model for digital mental health interventions poised to reshape clinical practice worldwide. Continued research and collaborative engagement among technologists, clinicians, and patients will be essential to realize the full potential of this promising innovation.
Subject of Research:
Development and usability evaluation of an audio-based cognitive behavioral therapy mobile app aimed at managing depression in hemodialysis patients.
Article Title:
Development and usability evaluation of an audio-based cognitive behavioral therapy mobile app for depression in hemodialysis patients.
Article References:
Narimanpour, F., Pirnejad, H., Makhdoomi, K. et al. Development and usability evaluation of an audio-based cognitive behavioral therapy mobile app for depression in hemodialysis patients. BMC Psychol (2025). https://doi.org/10.1186/s40359-025-03732-7
Image Credits: AI Generated