Antimicrobial resistance (AMR) stands as one of the most profound challenges in global public health, threatening decades of medical progress and imperiling modern healthcare systems. From the moment antimicrobial agents were first introduced therapeutically, an inevitable arms race began between these life-saving drugs and the ability of microorganisms to develop resistance. While antimicrobial resistance genes (ARGs) have existed naturally for millions of years across diverse environmental reservoirs, the unprecedented escalation of antimicrobial usage in human, animal, and environmental sectors over the past eight decades has dramatically reshaped the landscape of AMR emergence and spread.
The entanglement of antimicrobial resistance within and across the three intersecting domains of “One Health”—humans, animals, and the environment—amplifies the complexity of this crisis. Unlike classical infectious diseases limited to a single host or ecosystem, resistance genes traverse these boundaries continually, propelled by numerous direct and indirect pathways of transmission. These include not only clinical misuse and agricultural overuse of antimicrobials but also widespread contamination of environmental compartments such as water bodies and soils. This multifaceted connectivity of resistance determinants enhances the global burden of AMR and complicates containment efforts.
Historically, AMR genes evolved as natural defensive mechanisms amongst microbes competing for ecological niches. However, anthropogenic activities, particularly the prolific deployment of antimicrobials in medicine, farming, and aquaculture, have exponentially increased selective pressure that favors resistant strains. This selective amplification leads to the enrichment and mobilization of ARGs, facilitating horizontal gene transfer mechanisms among distinct bacterial populations. Mobile genetic elements such as plasmids, integrons, and transposons play a vital role in this genetic interplay, allowing ARGs to jump species barriers and spread rapidly in microbial communities.
One of the pivotal challenges lies in the environmental dimension of AMR dissemination. Aquatic environments, in particular, serve as dynamic reservoirs and conduits for resistance genes. Pollutants originating from human sewage discharge, agricultural runoff laden with antimicrobial residues, and industrial effluents create hotbeds for the proliferation and exchange of AMR determinants in natural water systems. These ecosystems, often understudied in antimicrobial resistance surveillance, represent crucial nodes where cross-sectorial transmission is facilitated, linking clinical, agricultural, and environmental settings.
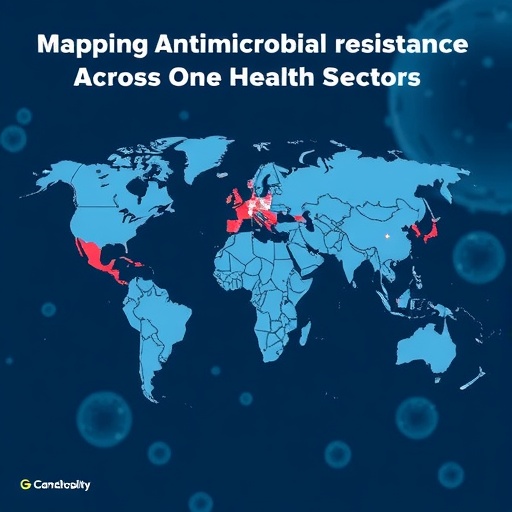
The concept of One Health places imperative emphasis on understanding AMR not merely as a clinical or agricultural problem but as a highly interconnected issue requiring integrated action. This framework calls for collaborative surveillance systems, data-sharing, and harmonized policy interventions encompassing human medicine, veterinary practices, and environmental management. However, despite widespread recognition of this interconnectedness, actual implementation of effective AMR National Action Plans remains suboptimal in many regions, particularly low- and middle-income countries where resource constraints, infrastructural deficits, and lack of technical expertise hinder comprehensive monitoring and control.
A major impediment to advancing global AMR control efforts is the insufficient elucidation of the connectivity patterns by which resistance genes move among the One Health sectors. This knowledge gap undermines the ability to target interventions strategically and hampers predictive modeling of AMR trajectories. Novel approaches leveraging high-throughput genomic and metagenomic technologies offer unprecedented resolution in deciphering these complex transmission networks. By sequencing microbial communities directly from diverse sources—wastewater, livestock environments, clinical samples—researchers can map ARG distributions, trace their origins, and identify critical transmission hotspots.
Metagenomics, in particular, circumvents the need to culture microbes, enabling comprehensive characterization of resistomes across entire ecosystems. This powerful tool can uncover ARGs harbored by uncultivable or rare bacterial populations, providing insights into hidden reservoirs and transmission vectors. Coupling genomic data with metadata on antimicrobial usage, environmental conditions, and host interactions allows for constructing integrative models that reveal the interplay between selective pressures and genetic mobility driving AMR dynamics.
Understanding AMR connectivity at the ecological level entails studying how microbial communities interact within environmental niches, shaping the selection and maintenance of resistance traits. At the microbial level, investigating the mechanisms facilitating horizontal gene transfer—including conjugation, transduction, and transformation—sheds light on how resistance genes migrate between species and genera. Meanwhile, at the genetic level, detailed analyses of ARG sequences, their genetic contexts, and associated mobile elements are critical for identifying evolutionary pathways and potential points of intervention.
Addressing AMR through the One Health lens also requires recognizing socio-economic and behavioral factors influencing antimicrobial use and environmental contamination. In many low-resource settings, lack of regulation, inadequate wastewater treatment, and unmonitored antibiotic sales contribute to uncontrolled antimicrobial exposure and resistance proliferation. Thus, combating AMR necessitates multi-sectoral policies encompassing improved stewardship, sanitation infrastructure enhancement, and public awareness campaigns tailored to local contexts.
International efforts aimed at halting AMR progression must prioritize integrated cross-sector studies that bridge human health, veterinary medicine, and environmental science. Such multidisciplinary research collaborations foster standardized methodologies, enabling comparability of data across regions and facilitating global surveillance networks. This harmonization is essential not only for tracking global trends but also for informing evidence-based regulatory strategies and fostering investments aligned with the global burden of antimicrobial resistance.
The urgency of this global health threat calls for enhanced funding and political commitment to support genomic and metagenomic research focused on AMR connectivity. Investments are needed to build capacity in regions vulnerable due to limited technical infrastructure, ensuring equitable participation in global surveillance efforts. Additionally, promoting open-access data platforms will accelerate knowledge exchange and empower policymakers to devise informed, adaptive responses.
Mitigating the spread of AMR demands innovative intervention strategies informed by connectivity insights. For instance, identifying critical control points within environmental reservoirs—such as wastewater treatment plants where ARG concentrations peak—can guide targeted mitigation measures, including advanced filtration technologies or bioremediation approaches. Similarly, modifying agricultural practices to reduce prophylactic antimicrobial use and improve animal husbandry can lower selective pressures that drive resistance emergence.
The integration of cutting-edge technologies with the One Health model holds promise for transforming AMR management from reactive containment to proactive prevention. Genomic surveillance offers real-time monitoring capabilities to detect emerging resistance mechanisms promptly and to evaluate intervention effectiveness over time. Through continuous data feedback loops, this dynamic approach can enable rapid adjustments in treatment guidelines, antimicrobial usage policies, and environmental management practices.
Ultimately, the fight against antimicrobial resistance is a race against time, requiring synchronized actions transcending disciplinary and geographical borders. Recognizing the fundamental role of connectivity in spreading resistance genes across human, animal, and environmental interfaces is paramount. By harnessing genomics and metagenomics as powerful tools to map these connections, and by fostering cross-sector collaborations, the global community can better anticipate, respond to, and contain the AMR threat.
In conclusion, antimicrobial resistance represents a multifaceted crisis shaped by the intricate interplay of genetic, microbial, and ecological factors within the One Health framework. Concerted efforts to understand and disrupt connectivity pathways underpin the future of AMR mitigation. As we stand on the cusp of genomic innovation and global cooperation, scaling up integrated surveillance and harmonized interventions offers a hopeful pathway toward safeguarding the effectiveness of antimicrobials for generations to come.
Subject of Research: Antimicrobial resistance (AMR) connectivity across humans, animals, and the environment within the One Health framework.
Article Title: Assessing antimicrobial resistance connectivity across One Health sectors.
Article References:
Li, L., Li, B., Yin, X. et al. Assessing antimicrobial resistance connectivity across One Health sectors. Nat Water (2025). https://doi.org/10.1038/s44221-025-00514-8
Image Credits: AI Generated