Intrauterine devices (IUDs) represent one of the most effective and widely used forms of long-term contraception worldwide. However, despite their high efficacy, some individuals hesitate or avoid IUD use due to apprehensions surrounding the insertion procedure. Fear of pain during IUD placement remains a notable barrier in clinical practice, leading researchers and practitioners to explore innovations aimed at reducing patient discomfort and improving procedural experience. A recent investigation addresses these concerns by comparing ultrasound-guided IUD insertion with conventional methods, focusing particularly on procedural duration and associated pain.
Traditional IUD placement often involves multiple steps, including a bimanual pelvic examination and uterine sounding, procedures which some patients find uncomfortable or distressing. The conventional approach requires clinicians to palpate the uterus and measure uterine depth manually to ensure proper device positioning. While effective, this approach can extend the procedure time and potentially increase discomfort due to the invasiveness of these preliminary assessments. The integration of ultrasound guidance into the insertion protocol presents an opportunity to revisit these standard practices through a technological lens, aiming for enhanced precision and patient comfort.
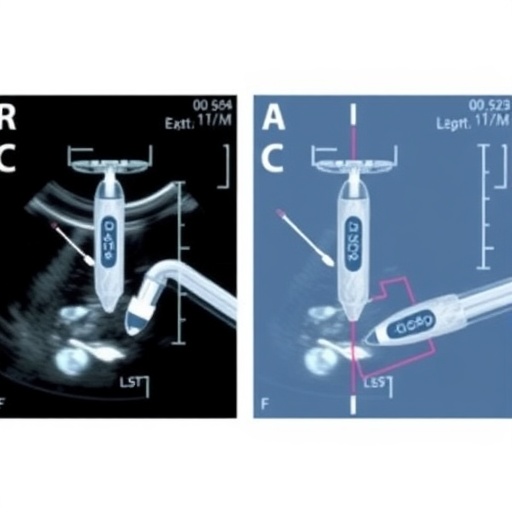
In the ultrasound-guided approach, clinicians utilize transabdominal ultrasound imaging to visualize the anatomy of the uterus directly. This non-invasive imaging modality allows for direct measurement of the distance from the cervix to the uterine fundus, providing real-time spatial data that inform device placement. Ultrasound confirmation of IUD positioning after insertion ensures accurate localization, potentially reducing the likelihood of malposition and its associated complications. Notably, this method eliminates the need for uterine sounding and bimanual pelvic examinations, theoretically reducing procedural invasiveness.
The study was conducted in a family medicine teaching health center environment, enrolling a total of 47 patients who were assigned either to the ultrasound-guided IUD insertion group or the conventional method group. In the ultrasound-guided cohort, the procedure was conducted with real-time imaging support by clinicians trained in point-of-care ultrasound (POCUS) or obstetrics and gynecology, while in the conventional group, resident physicians performed the standard pre-insertion assessments. Pain was quantified immediately following device placement using a visual analog scale ranging from zero to ten, and total procedure time was meticulously recorded in seconds, offering quantitative data for comparative analysis.
One of the study’s most compelling findings was that ultrasound-guided IUD insertion significantly reduced procedure time compared to the conventional method. The real-time visualization eliminated the need for multiple manual measures, streamlining the process into a more efficient operation. This reduction in procedural duration may translate into increased throughput in clinical settings, improving workflow and resource utilization while minimizing patient discomfort associated with prolonged procedures.
Contrary to what might be expected, the study demonstrated no significant difference in pain scores between the ultrasound-guided and conventional insertion groups. Despite the ultrasound method bypassing potentially uncomfortable manual maneuvers such as uterine sounding, patients’ subjective pain experience remained comparable. This insight challenges assumptions that procedure time reduction and less invasive preparatory steps would necessarily reduce pain perception, suggesting that other factors may influence pain during IUD insertion.
An additional notable outcome was the lack of correlation between procedure time and pain levels reported by patients. This dissociation indicates that a shorter procedural duration does not inherently guarantee less pain. Pain perception is complex and can be affected by multiple variables, including individual pain thresholds, anxiety, procedural technique, and clinician experience. Therefore, while ultrasound guidance optimizes efficiency, it does not singularly dictate the patient’s pain experience.
The clinical implications of these findings are multifaceted. By adopting ultrasound guidance, practitioners may benefit from enhanced procedural efficiency without compromising patient comfort. The reduced time of insertion could enable clinics to accommodate more patients or allocate time to other critical care activities. Moreover, the ability to visualize uterine anatomy dynamically may provide additional reassurance for clinicians in challenging cases, such as patients with atypical uterine positioning or history of difficult insertions.
From a technological perspective, the study highlights the growing role of point-of-care ultrasound (POCUS) beyond traditional diagnostic applications. Incorporating ultrasound into routine gynecological procedures epitomizes the broader trend of leveraging imaging technology to refine and enhance clinical workflows. As POCUS devices become increasingly affordable, portable, and user-friendly, their integration into outpatient settings is likely to expand, improving procedural accuracy across multiple disciplines.
Despite the promising advantages of ultrasound-guided insertion, practitioners should be aware that proficiency with POCUS is critical. Interpretation of images and navigation require specific training to avoid misplacement errors. The study involved supervised family-medicine residents working alongside ultrasound-trained physicians or OB-GYNs, reflecting a model where interdisciplinary collaboration and mentorship may optimize patient outcomes.
Importantly, while the sample size was limited to 47 participants across two groups, the findings open avenues for larger-scale investigations. Future research could explore additional patient-centered outcomes such as anxiety reduction, satisfaction, and long-term retention of the IUD. It would also be beneficial to evaluate cost-effectiveness analyses comparing ultrasound-guided and conventional insertion techniques to guide health policy decisions.
In summary, ultrasound-guided IUD insertion emerges as an innovative approach that streamlines procedure time without adversely affecting pain levels. The capability to bypass pelvic examination and uterine sounding offers a less invasive pathway bolstered by real-time imaging accuracy. While pain reduction was not realized in this study, procedural efficiency gains present meaningful benefits to healthcare delivery. This study thus underscores the potential of integrating ultrasound technology into family medicine and gynecological practice to improve clinical workflows and patient care.
Given the growing emphasis on patient-centered care and minimally invasive procedures, technologies that complement traditional methods are increasingly relevant. This study exemplifies how medical innovation does not always manifest as reduced discomfort but can excel by optimizing resource use and clinician confidence. Ultrasound-guided IUD insertion may become an exemplar of such innovation, fostering more efficient and precise family medicine procedures in the future.
Subject of Research: Ultrasound guidance versus conventional IUD insertion methods.
Article Title: Ultrasound Guidance Compared With Conventional Methods Reduces IUD Insertion Time.
News Publication Date: 22-Sep-2025.
Web References: https://www.annfammed.org/content/23/5/460
Keywords: Family medicine, Female fertility, Human reproduction, Ultrasonics.