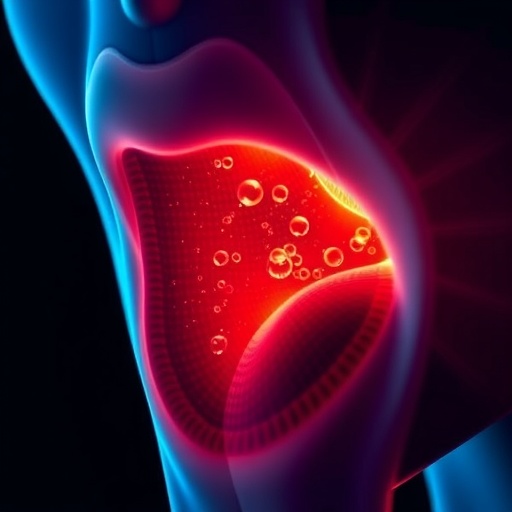
Recent studies have showcased a critical advancement in the field of healthcare for individuals living with HIV, particularly concerning the treatment of anal high-grade squamous intraepithelial lesions (HSIL). New insights reveal that proactive treatment of these lesions significantly reduces the risk of progression to invasive anal cancer. This breakthrough is particularly vital as anal cancer holds a higher incidence among HIV-positive individuals, making preventive strategies essential for enhancing patient outcomes. The work conducted by Allon, Alexander, and Terndrup, published in the Journal of General Internal Medicine, sheds light on this increasingly important issue.
In the context of HIV, the immune system is compromised, leaving patients vulnerable to various infections and cancers. Among those risks, anal squamous cell carcinoma stands out due to its increased prevalence in this population. Understanding the biological mechanisms behind this heightened risk is crucial to developing effective intervention strategies. The research highlights how high-grade lesions can serve as precursors to invasive cancer, emphasizing the need for early detection and treatment.
The study employed a robust set of methodologies, incorporating both clinical data and observational research to identify the links between the management of HSIL and cancer progression. The researchers meticulously analyzed patient outcomes over time, providing compelling evidence that timely intervention plays a vital role in preventing the onset of anal cancer. These findings not only provide a basis for clinical practice but also pave the way for further research in this domain.
Turning to the specifics of the findings, the researchers observed a striking reduction in the rates of invasive anal cancer among those treated for HSIL as compared to unscreened individuals. This results signify a significant leap in preventive measures that can be easily implemented in healthcare settings. By focusing on early treatment, the healthcare community can potentially diminish the likelihood of developing a life-threatening condition that burdens many HIV-positive patients.
Additionally, the authors addressed the broader implications of their findings in regards to public health policies. They advocate for increased awareness and screening programs tailored specifically for vulnerable populations, particularly those living with HIV. By establishing guidelines that foster early diagnosis and intervention, healthcare providers can bridge the gap between risk and effective management, significantly improving life expectancy and quality of life for their patients.
Equally critical is the discussion on healthcare accessibility and education. Many individuals living with HIV may not be aware of the risks associated with anal HSIL or the preventive options available. This underlines the necessity for community outreach and education efforts to ensure patients understand their health status and the importance of regular screenings. The researchers emphasize that healthcare systems must prioritize educational initiatives that inform patients about the link between HIV, HSIL, and anal cancer.
Another key aspect discussed in the study is the role of healthcare providers in delivering patient-centered care. Physicians must be equipped not only with the knowledge of these conditions but also with the sensitivity required to communicate the risks effectively. Establishing open lines of communication fosters trust, empowering patients to engage proactively with their health. This is particularly relevant in populations that may experience stigma or fear surrounding their HIV status.
As researchers strive towards enhancing patient outcomes, they also point to the promising area of immunotherapy treatment options for high-grade lesions. By harnessing the body’s immune response, these treatments could offer a robust avenue for combating not only existing lesions but also the potential for malignant transformation. This avenue of exploration is still in its infancy, yet it opens up exciting possibilities for future research and clinical practices.
Furthermore, ongoing studies must address the long-term sustainability of current treatment protocols. Will the benefits observed in short-term analyses hold true over decades? Are there potential side effects or complications that could arise from aggressive treatments? Monitoring these factors will be essential to ensuring that the healthcare community can provide comprehensive and holistic management strategies for HIV-positive patients.
The landscape of HIV treatment is continuously evolving, shaped by ongoing research like that undertaken by Allon and colleagues. As healthcare providers embrace innovative approaches to managing HSIL and associated risks, they must not lose sight of the multidimensional challenges faced by individuals living with HIV. Fostering a holistic approach that encompasses mental health, social support, and regular medical care is paramount to achieving optimal patient outcomes.
In summary, the groundbreaking study underscores the necessity of addressing anal high-grade squamous intraepithelial lesions as a key public health concern. By implementing early detection and treatment protocols, healthcare providers can significantly impact the lives of individuals with HIV. With an emphasis on education and accessibility, stakeholders can establish pathways that lead to better health outcomes, ultimately reducing the incidence of invasive anal cancer where it matters most. The call to action resonates loudly; the time for change in healthcare practices is now.
The importance of these findings transcends the individual patient level, signaling a shift towards more proactive health strategies within at-risk populations. By utilizing insights derived from this research, healthcare professionals can better inform their strategies and protocols, elevating the standard of care provided to those living with HIV. The implications are vast, promising a brighter future for countless individuals who rely on effective management of their health to lead fulfilling lives.
The research illustrates a hopeful advance in the fight against cancer in HIV-positive populations, a reminder that with continued efforts, strides can be made toward a future where HIV is no longer a life-limiting condition, and associated risks are managed effectively. Each new study, such as the one by Allon and colleagues, not only contributes to the scientific tapestry of knowledge but also has the power to transform lives.
As healthcare professionals digest and implement these findings, we stand at the precipice of a new era in HIV treatment—one defined by informed choices, early interventions, and the relentless pursuit of improved patient outcomes.
Subject of Research: Treatment of anal high-grade squamous intraepithelial lesions in HIV-positive patients to reduce progression to anal cancer.
Article Title: EBM BLS: Treating Anal High-grade Squamous Intraepithelial Lesions Reduces Progression to Invasive Anal Cancer in People Living with HIV.
Article References:
Allon, S., Alexander, J.T. & Terndrup, C. EBM BLS: Treating Anal High-grade Squamous Intraepithelial Lesions Reduces Progression to Invasive Anal Cancer in People Living with HIV.
J GEN INTERN MED (2025). https://doi.org/10.1007/s11606-025-09828-5
Image Credits: AI Generated
DOI:
Keywords: HIV, anal high-grade squamous intraepithelial lesions, anal cancer, treatment, prevention.