In a pioneering leap forward in pediatric traumatic brain injury (TBI) research, a new study published in Pediatric Research unveils the potential of aptamer-based proteomics to revolutionize diagnostics and treatment paradigms. This innovative pilot study delves into the molecular intricacies of severe brain injuries in children, illuminating how cutting-edge proteomic technologies can decode complex biological responses and potentially guide personalized medical interventions.
Traumatic brain injury remains a leading cause of morbidity and mortality in pediatric populations worldwide. Despite advances in clinical care, the intricate pathophysiological processes triggered by TBI often elude comprehensive characterization, complicating prognosis and treatment. Traditional diagnostic methods largely rely on imaging and clinical assessment, which, while invaluable, offer limited insights into the underlying molecular events shaping each patient’s unique injury trajectory. This knowledge gap underscores the urgent need for more precise, biomolecular tools that can unravel the proteomic alterations induced by trauma.
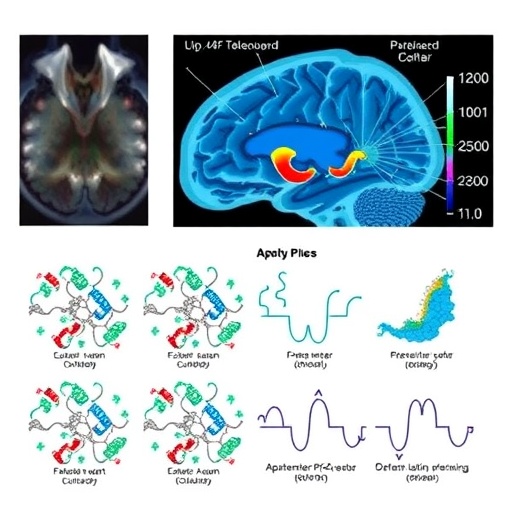
Enter aptamer-based proteomics—a technological breakthrough harnessing the specificity and sensitivity of aptamers, which are short, single-stranded oligonucleotides that bind proteins with extraordinary precision. Unlike conventional antibodies, aptamers are synthetically engineered, enabling them to target a broader array of proteins with remarkable stability and scalability. This technology facilitates the high-throughput quantification of thousands of proteins simultaneously, mapping the proteomic landscape in exceptional detail. The adoption of aptamer-based methods in pediatric TBI research offers a powerful new lens to understand how protein expression and interactions evolve after injury.
The study spearheaded by De Souza et al. embarks on an ambitious exploration of this proteomic frontier, enrolling pediatric patients with severe TBI and analyzing their plasma proteomes using an aptamer-based platform. Their approach is both comprehensive and nuanced, aiming to identify protein biomarkers that are not only elevated or suppressed following brain trauma but also functionally relevant to injury mechanisms such as inflammation, cell death, and tissue repair. These biomarkers have the potential to serve as early indicators of injury severity and predictors of long-term outcomes.
Critical to the success of this investigation is the study’s rigorous design, leveraging the high sensitivity of aptamer arrays to detect subtle protein expression changes that conventional assays might overlook. By profiling over a thousand proteins simultaneously, the researchers revealed distinctive signatures correlated with different stages and severities of TBI. This multiplex capability transforms proteomics from a mere inventory exercise into a predictive and dynamic tool, capable of guiding critical clinical decisions in real time.
Moreover, aptamer-based proteomics offers unparalleled reproducibility and affordability compared to mass spectrometry, positioning it as a highly scalable solution for clinical translation. Given the urgent need for point-of-care diagnostics in pediatric intensive care units, this technological innovation bridges the gap between bench discovery and bedside application. It also opens avenues for monitoring therapeutic responses and adapting interventions to individual molecular profiles, thereby ushering in the era of precision medicine in pediatric neurotrauma.
Importantly, the study uncovers previously unappreciated protein networks linked to neuroinflammation and neuroprotection, suggesting that TBI triggers complex cascades that can either exacerbate damage or foster recovery depending on temporal and molecular contexts. Understanding these networks at a proteomic level enables researchers and clinicians to pinpoint new drug targets and to develop biomarker panels that inform tailored treatment strategies, minimizing secondary injury while maximizing neuronal survival.
In addition to biomarker identification, the study highlights the role of systemic responses to brain injury. Pediatric TBI does not simply affect neural tissue in isolation; it instigates systemic immune activation and metabolic shifts which can be quantitatively tracked through proteomic changes in circulating plasma proteins. These insights foster a holistic understanding of trauma pathology, linking neurological damage with peripheral physiological adaptations and complications.
This pilot study also exemplifies the collaborative spirit driving cutting-edge biomedical research. Integrating expertise from neurobiology, proteomics, computational biology, and pediatric critical care, the team deployed advanced bioinformatics pipelines to interpret the massive datasets generated. Their integrative analysis unearthed meaningful correlations between proteomic patterns and clinical phenotypes, showing promise for developing algorithms that predict patient trajectories with unprecedented accuracy.
From a translational perspective, the implications of these findings are profound. Early and precise proteomic profiling could empower clinicians to stratify patients into risk categories, tailor therapeutic regimens, and monitor recovery or secondary complications more effectively. Such capabilities could transform the prognosis for children suffering severe TBI, who currently face uncertain outcomes and limited options. Moreover, this study sets the stage for larger-scale validations and longitudinal analyses that can refine proteomic signatures and validate their clinical utility.
Technologically, the robustness of aptamer-based assays supports their integration into future multi-omic studies, combining proteomics with genomics, metabolomics, and transcriptomics to generate comprehensive molecular portraits of injury. This systems biology approach is key to unraveling the multifaceted nature of brain trauma, revealing interactions across biological layers that determine clinical outcomes. As the technology matures, it may facilitate non-invasive monitoring through peripheral fluids, reducing the need for invasive procedures in vulnerable pediatric patients.
Finally, the study calls attention to ethical considerations and the need for careful implementation of molecular diagnostics in pediatric care. While aptamer-based proteomics heralds a paradigm shift, clinical adoption must be accompanied by rigorous validation, standardization, and sensitivity to patient and family concerns. The promise of personalized medicine must be balanced with equitable access, data privacy, and informed consent, particularly in the context of vulnerable pediatric populations.
In summary, this groundbreaking pilot study not only illuminates the complex proteomic changes following severe pediatric traumatic brain injury but also champions aptamer-based proteomics as a transformative clinical tool. Its capacity to decode hundreds of protein alterations simultaneously lays a foundation for targeted diagnostics and personalized therapeutics, ultimately aiming to improve survival and quality of life for children affected by devastating brain injuries. As research accelerates, this innovative approach holds the potential to redefine pediatric neurotrauma care for years to come.
Subject of Research:
Proteomic profiling using aptamer-based technology in pediatric patients with severe traumatic brain injury.
Article Title:
Aptamer-based proteomics in pediatric patients with severe traumatic brain injury: a pilot study.
Article References:
De Souza, B.J., Wolf, M.S., Leonard, J.R. et al. Aptamer-based proteomics in pediatric patients with severe traumatic brain injury: a pilot study. Pediatr Res (2026). https://doi.org/10.1038/s41390-026-04798-8
Image Credits: AI Generated
DOI: 19 February 2026