The persistent overexpression of the lysine-specific demethylase 1 (LSD1) enzyme has been notoriously linked to poor clinical outcomes across a spectrum of malignancies. This correlation underscores the critical need for innovative therapeutic strategies targeting LSD1, which remains a compelling target given its pivotal role in modulating histone methylation patterns and regulating gene expression in cancer cells. Historically, the development of small-molecule inhibitors against LSD1 has encountered formidable obstacles, primarily hindered by toxicities that limit dosing and unintended interactions with non-target proteins. These limitations have stymied the clinical progression of such inhibitors, driving researchers to seek new modalities that can circumvent these pharmacological pitfalls.
Enter PROTAC (Proteolysis Targeting Chimera) technology, a transformative approach that diverges fundamentally from traditional inhibition by harnessing the cell’s own ubiquitin-proteasome system to selectively degrade the LSD1 enzyme. PROTAC molecules operate catalytically, tethering the target protein to an E3 ubiquitin ligase which flags it for destruction. This elegant mechanism ensures profound and durable depletion of LSD1 at lower compound concentrations compared to occupancy-driven inhibitors. Such catalytic degradation promises not only heightened efficacy but also reduced emergence of drug resistance and diminished off-target toxicities, positioning PROTACs as a next-generation therapeutic platform in oncology.
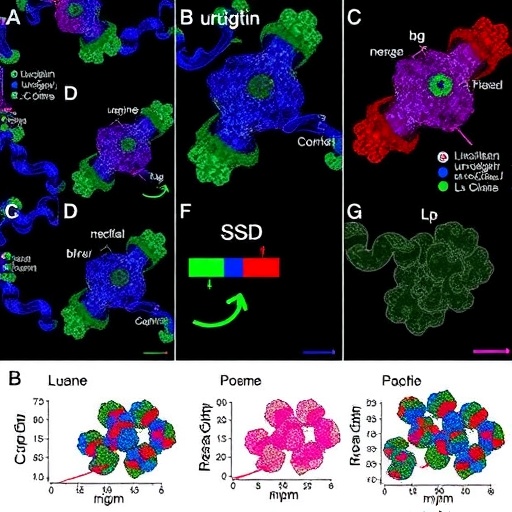
In this groundbreaking study, the research team engineered a series of PROTAC compounds by fusing an LSD1-binding moiety named LI-1 with the cereblon (CRBN)-recruiting ligand thalidomide via linkers of varying lengths. Through meticulous structure-activity relationship (SAR) investigations, a candidate designated LD-110 surfaced as the most potent and selective degrader of LSD1. Biochemical assays revealed that LD-110 substantially diminished LSD1 protein levels in breast and lung cancer cell lines in both a time-dependent and dose-dependent fashion. Notably, the half-maximal degradation concentrations (DC₅₀) of LD-110 were impressively low in MDA-MB-231 and MDA-MB-453 breast cancer cells, registering at 9.54 and 7.08 nanomolar, respectively. Although lung cancer H520 cells exhibited a higher DC₅₀ of 446 nanomolar, this still represents significant efficacy given the challenge of targeting non-hematological tumors.
Validation of the underlying degradation mechanism was achieved through rigorous control experiments. The authors demonstrated that the proteasome inhibitor MG132 and the neddylation inhibitor MLN4924 effectively abrogated LD-110-induced LSD1 degradation, confirming the critical involvement of the ubiquitin-proteasome system and the CRBN E3 ligase pathway. Furthermore, competitive inhibition with the LI-1 warhead and thalidomide ligand prevented degradation, and a methylated analog of LD-110 (LD-110Me), incapable of binding CRBN, failed to induce either LSD1 degradation or downstream substrate accumulation. These findings collectively solidify that LD-110 functions as a bona fide PROTAC, exploiting CRBN recruitment to catalyze targeted proteostasis.
Beyond biochemical validation, the anti-proliferative effects of LD-110 were striking. The compound exhibited potent growth inhibition across diverse cancer cell lines, yielding half-maximal inhibitory concentrations (IC₅₀) ranging broadly but often in the sub-micromolar range. Of equal importance, pharmacokinetic profiling demonstrated that LD-110 possesses favorable in vivo characteristics, including bioavailability and metabolic stability, which translated into marked tumor growth suppression in both breast and lung cancer xenograft models. Remarkably, this potent anti-tumor activity was achieved without detectable systemic toxicity, suggesting an attractive therapeutic window for further development.
Delving into the mechanistic underpinnings of LD-110’s cytotoxicity revealed a sophisticated orchestration of cellular stress pathways. LD-110 was found to induce apoptotic cell death primarily via triggering endoplasmic reticulum (ER) stress, converging on activation of the ATF4-CHOP axis—a central regulator of stress-induced apoptosis. On one hand, transcriptional modulation stems from LSD1 degradation leading to increased H3K4 dimethylation (H3K4me2), which facilitates ATF4 gene expression. On the other hand, LD-110 also stimulates reactive oxygen species (ROS) production resulting in DNA damage, which activates the GCN2-eIF2α pathway to augment translational synthesis of ATF4 protein. This dual mechanism synergistically amplifies ATF4 levels, engaging downstream apoptotic effectors.
The ATF4-CHOP pathway modulates critical determinants of cell fate by rebalancing members of the BCL-2 protein family. Specifically, LD-110 elevates the expression of NOXA, a potent pro-apoptotic factor, while concomitantly reducing MCL1, an anti-apoptotic protein that often confers resistance to cell death. This shift in protein equilibrium decisively steers cancer cells toward programmed apoptosis, underpinning the robust anticancer effects observed.
Nonetheless, the use of CRBN as the E3 ligase recruitment element inherently carries limitations related to off-target degradation. CRBN naturally targets substrates such as GSPT1 and the IKZF family, which are not the intended therapeutic targets. Consistent with this, LD-110 also promoted degradation of GSPT1 alongside LSD1. Intriguingly, the researchers discovered that GSPT1 competes with LSD1 for LD-110 binding, thereby diminishing the degrader’s efficiency toward LSD1. Through siRNA-mediated knockdown of GSPT1, the inhibitory effect on LSD1 degradation was alleviated, resulting in enhanced LD-110 potency and more pronounced growth inhibition of cancer cells.
This observation suggests a compelling therapeutic strategy: combining LD-110 with a selective GSPT1 degrader could yield synergistic anti-tumor activity through dual pathway engagement. Such a combination may allow for dose reduction, potentially minimizing toxicity while maximizing efficacy—an elegant example of precision polypharmacology.
In summation, this investigation heralds LD-110 as a pioneering PROTAC molecule that effectively depletes LSD1, exhibiting significant anticancer activity in vitro and in vivo. The dual mechanism of inducing ER stress and modulating epigenetic marks represents a novel therapeutic angle to combat cancers characterized by LSD1 overexpression. With favorable pharmacokinetic and safety profiles, LD-110 stands poised as a promising candidate to advance into clinical development, potentially transforming the therapeutic landscape for patients afflicted with breast, lung, and possibly other cancers.
As the field of targeted protein degradation continues to revolutionize drug discovery, studies such as this provide compelling proof-of-concept that PROTACs can surpass the limitations of traditional inhibitors. By capitalizing on polyfunctional molecular design, researchers are opening avenues toward durable, selective, and potent cancer therapies that exploit intrinsic cellular machinery to disarm oncogenic drivers.
Future research will undoubtedly explore further optimization of linker chemistry, E3 ligase selection, and combination regimens with other targeted agents. Moreover, deciphering and mitigating off-target effects inherent to PROTAC technology remains a priority to maximize clinical benefit. The promising results reported here pave the way for a new era in epigenetic cancer therapy, leveraging protein degradation machinery to deliver precise, potent, and lasting tumor suppression.
Subject of Research: LSD1 Protein Degradation Using PROTAC Technology for Cancer Therapy
Article Title: Discovery of LD-110 as a Potent PROTAC Degrader of LSD1 with Therapeutic Efficacy in Breast and Lung Cancer Models
Web References:
10.1016/j.scib.2025.10.024
Keywords:
Life sciences, Health and medicine, Biochemistry, Cancer treatments