In a groundbreaking advance that promises to reshape our understanding of schizophrenia, researchers have unveiled new insights into the complex dysfunction of dopamine subsystems within the brain, employing an innovative PET meta-analysis approach. This study meticulously dissects the heterogeneity of dopamine activity in schizophrenia, offering unprecedented clarity into the varied nature of this psychiatric disorder that has puzzled neuroscientists for decades.
Dopamine, a neurotransmitter fundamental to brain function, has long been linked to schizophrenia, a condition marked by profound disruptions in thought, perception, and behavior. Traditional views largely treated dopamine dysfunction as a uniform phenomenon; however, this expansive meta-analysis reveals a far more intricate tapestry of dysfunctions across different dopamine subsystems. The implications for both diagnostic precision and therapeutic strategy are profound, opening up a pathway towards more personalized and effective interventions.
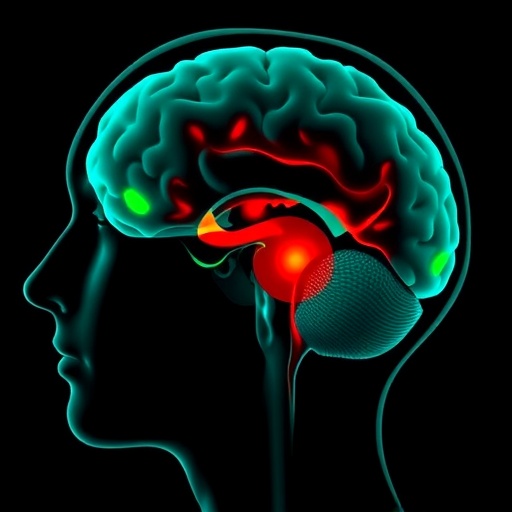
Leveraging positron emission tomography (PET), a sophisticated imaging modality that allows researchers to observe neurotransmitter dynamics in the living brain, the study amalgamated data from multiple PET studies to generate a high-resolution map of dopaminergic activity across distinct brain regions implicated in schizophrenia. By synthesizing this wealth of data, the analysis established striking regional differences in dopamine transmission patterns, contesting the notion of a one-size-fits-all dopamine deficit in schizophrenia.
The researchers focused on disentangling dysfunction across key dopamine pathways, including the mesolimbic, mesocortical, and nigrostriatal systems. Each of these subsystems plays a specialized role in cognition, motivation, and motor control, respectively. The meta-analysis documented that hyperactivity is predominant in the mesolimbic pathway, often linked to the manifestation of psychotic symptoms such as hallucinations and delusions. In stark contrast, reduced dopamine function was observed in the mesocortical pathway, correlating with negative symptoms such as social withdrawal and cognitive impairment.
This refined perspective is crucial because it moves away from the monolithic view of dopamine dysregulation toward recognizing that schizophrenia’s symptomatology may arise from differential patterns of dopaminergic dysfunction within discrete neural circuits. Such differentiation could explain why some patients respond robustly to dopamine antagonists—primarily ameliorating psychosis—while others exhibit persistent negative and cognitive symptoms that remain resistant to current treatments.
The study further interrogates the temporal dynamics of dopamine dysfunction, signalling that these abnormalities are not static but evolve throughout the course of the illness. Early stages of schizophrenia showed more pronounced mesolimbic hyperdopaminergia, while chronic stages featured exacerbated mesocortical hypodopaminergia. This temporal heterogeneity aligns with clinical observations about symptom progression and treatment response variability, underscoring the need for stage-specific therapeutic approaches.
Importantly, the meta-analytic framework addressed the methodological variability that has previously hampered clear interpretations of PET studies in schizophrenia. By standardizing measures across studies and employing rigorous statistical models, the research team minimized biases and enhanced the reproducibility of findings. This methodological strength establishes a new benchmark for neuroimaging meta-analyses in psychiatry and could be adapted for other neurotransmitter research paradigms.
Beyond the identification of dopamine dysfunction patterns, the findings carry substantial implications for drug development. Current antipsychotics predominantly target mesolimbic dopamine receptors, but emerging evidence from this study suggests that augmenting mesocortical dopamine function might represent a pivotal strategy for alleviating cognitive and negative symptoms, which are notoriously difficult to treat. This dual-target hypothesis could revolutionize pharmacological interventions by promoting the development of novel compounds capable of finely modulating dopamine subsystems.
The insights gained extend into the realm of precision psychiatry, heralding an era where clinicians could tailor treatments based on individual dopaminergic profiles elucidated via PET imaging or proxy biomarkers. This would transform the clinical landscape from empiric treatment trials to mechanism-based interventions with greater likelihoods of success and fewer adverse effects. Personalized therapeutic regimens could drastically improve quality of life for millions affected by schizophrenia worldwide.
Moreover, this study paves the way for exploring how dopamine subsystem dysfunction intersects with other neurotransmitter systems implicated in schizophrenia, such as glutamate and GABA. Understanding these complex inter-system relationships could illuminate the broader neurochemical framework of this disorder and foster multi-targeted treatment regimens combining dopaminergic modulation with other neural substrates.
The research also underlines the significance of neurodevelopmental trajectories in determining dopamine subsystem integrity. Genetic and environmental risk factors influencing brain development may predispose individuals to distinct dopamine dysfunction patterns, contributing to the heterogeneity observed in clinical presentations. Future investigations building on this meta-analysis will be essential to decipher the etiological origins of dopamine abnormalities and their interactions with neurodevelopmental processes.
Clinical translation of these findings will necessitate advancements in PET technology and the identification of affordable, non-invasive biomarkers that accurately reflect subsystem-specific dopamine function. Integrating PET-based measures with emerging modalities such as single-photon emission computed tomography (SPECT) and magnetic resonance spectroscopy (MRS) could enhance diagnostic accuracy and deepen our understanding of dopamine’s role in schizophrenia.
This meta-analysis not only challenges existing paradigms but also empowers the psychiatric research community to reconceptualize dopamine dysfunction in schizophrenia as a multidimensional, dynamic phenomenon. It encourages a shift from generalized to finely granulated neurobiological models, urging stakeholders in academia, pharmaceutical industries, and clinical practice to reconsider approaches to diagnosis, therapy, and research.
Ultimately, the study represents a significant stride towards resolving one of psychiatry’s most enduring puzzles. By illuminating the heterogeneous nature of dopamine dysfunction across subsystems, it opens fertile ground for innovations in treatment that hold the promise of greater efficacy, fewer side effects, and improved outcomes for those living with schizophrenia.
This vital research underscores the power of meta-analytic techniques to distill clarity from complexity and exemplifies how interdisciplinary collaboration—melding neuroimaging, psychiatry, and computational analysis—can propel the field forward. The dopamine subsystems’ nuanced dysfunction narrative revealed here marks a watershed moment, urging the global neuroscience community to embrace a more sophisticated understanding of mental illness.
As the dopamine story in schizophrenia unfolds with this new clarity, the prospect of more nuanced, targeted, and life-changing interventions grows tantalizingly closer. This work provides not only a scientific beacon but also a hopeful path forward, affirming that meticulous research can unlock the intricate mysteries of the human brain and transform the landscape of psychiatric care.
Subject of Research: Dopamine subsystem dysfunction heterogeneity in schizophrenia, investigated through positron emission tomography (PET) meta-analysis.
Article Title: Resolving the heterogeneity of dopamine subsystems dysfunction in schizophrenia: a PET meta-analysis.
Article References:
Zhao, Z., Li, X., Xie, Y. et al. Resolving the heterogeneity of dopamine subsystems dysfunction in schizophrenia: a PET meta-analysis. Schizophr 11, 139 (2025). https://doi.org/10.1038/s41537-025-00684-0
Image Credits: AI Generated