In a groundbreaking study that pushes the boundaries of our understanding of treatment-resistant schizophrenia, researchers have unveiled compelling evidence highlighting the intricate interplay between GABAergic inhibition and glutamatergic facilitation in the brains of afflicted patients. This investigation, employing state-of-the-art transcranial magnetic stimulation (TMS) alongside comprehensive clinical and cognitive assessments, sheds light on the neurophysiological mechanisms underlying one of psychiatry’s most challenging conditions.
Schizophrenia, a debilitating neuropsychiatric disorder characterized by hallucinations, delusions, and cognitive impairments, often defies conventional pharmacological interventions, particularly in its treatment-resistant forms. The study spearheaded by Barone, Senerchia, De Simone, and their colleagues sets out to unravel the neurochemical underpinnings of this resistance by focusing on two primary neurotransmitter systems: the gamma-aminobutyric acid (GABA) system, responsible for inhibitory signaling, and the glutamate system, which mediates excitatory signals in the brain.
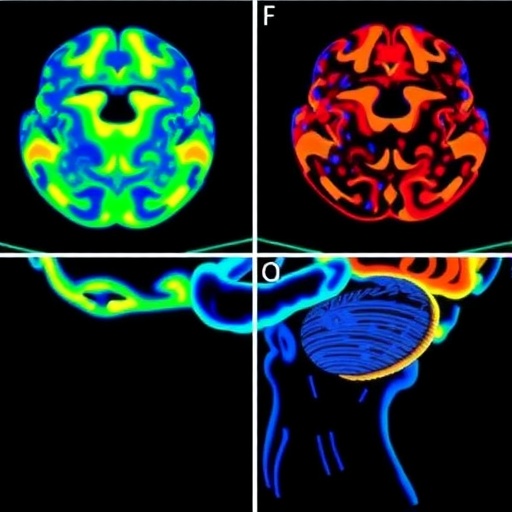
Central to this research is the use of TMS, a non-invasive brain stimulation technique that enables precise probing and modulation of cortical excitability in vivo. By integrating TMS with concurrent clinical and cognitive evaluations, the researchers devised a novel framework to simultaneously assess GABAergic inhibition and glutamate facilitation in patients who do not respond adequately to existing antipsychotic therapies. This multidimensional approach marks a significant departure from traditional methods relying solely on clinical symptomatology or neurochemical assays performed post-mortem.
Across numerous TMS protocols, the team explored inhibitory and facilitatory cortical circuits, with a particular emphasis on short-interval intracortical inhibition (SICI) and intracortical facilitation (ICF), known proxies for GABA_A and glutamate NMDA receptor-mediated activity, respectively. Their findings illuminate a dysregulation characterized by markedly diminished GABAergic inhibition coupled with aberrantly augmented glutamatergic facilitation. This imbalance potentially contributes to the persistent positive and cognitive symptoms observed in treatment-resistant cases.
The authors also documented correlations between these neurophysiological metrics and clinical severity scales, demonstrating that reduced inhibitory tone associates strongly with exacerbated symptomatology, while increased excitatory processes may underpin cognitive deficits, such as impaired working memory and executive function. These multidimensional insight pave the way for biomarkers that could stratify patients according to neurochemical profiles, thereby guiding precision medicine approaches in schizophrenia care.
More intriguingly, the study highlighted the plasticity potential of these circuits, suggesting that targeted interventions aiming to restore GABA-glutamate homeostasis could ameliorate symptoms and overcome pharmacoresistance. This perspective aligns with emerging therapeutic paradigms favoring neuromodulation and receptor-specific pharmacotherapies over broad dopamine antagonism alone.
By combining rigorous quantitative neurophysiology with clinical phenotyping, this research challenges the dopamine-centric framework long dominant in schizophrenia research and treatment. Instead, it posits that aberrations in intrinsic cortical excitability, governed through a delicate balance of inhibitory and excitatory neurotransmission, play a foundational role in the pathophysiology of treatment resistance.
Furthermore, the implementation of TMS as both a diagnostic and potentially therapeutic tool enriches the clinical toolkit, offering avenues for real-time monitoring of neurochemical dynamics in individual patients. This could revolutionize the way clinicians adapt and personalize therapeutic regimens, moving beyond the trial-and-error approaches currently prevalent.
Another notable aspect of the study is its integration of cognitive assessments alongside neurophysiological measures. By mapping excitatory/inhibitory imbalances to specific domains of cognitive dysfunction, the researchers underscore the functional relevance of these findings, extending beyond symptom control to enhancing quality of life and day-to-day cognitive performance in patients.
The methodology detailed in the paper demonstrates remarkable rigor, with careful control groups and longitudinal monitoring, which strengthens the validity of conclusions regarding the stability and state-dependence of cortical excitability measures. This is crucial given the fluctuating course of schizophrenia and the impact of external factors such as medication changes and environmental stressors.
In summary, this pioneering investigation offers a comprehensive in vivo map of GABAergic and glutamatergic function in treatment-resistant schizophrenia. It paves the path toward a new neurochemical framework that may redefine diagnostic criteria, therapeutic targets, and clinical outcome measures. The promise of this research lies not only in its immediate findings but in stimulating further exploration into tailored neuromodulatory therapies, potentially revolutionizing care for one of psychiatry’s most intractable disorders.
The implications for future research are profound. Follow-up studies may explore the effects of novel pharmacological agents that specifically enhance GABAergic transmission or modulate glutamate receptor activity, assessed via the robust TMS-based protocols validated here. Parallel efforts could refine patient stratification models using neurophysiological markers to predict treatment responsiveness with greater accuracy.
Moreover, the study invites reconsideration of how psychiatric disorders fundamentally manifest at the circuitry level, encouraging interdisciplinary collaborations between neuroscientists, psychiatrists, and neuroengineers. This research exemplifies the power of integrating cutting-edge neurotechnology with clinical insight to drive forward the frontier of mental health care.
In an era where mental health remains a critical global challenge, this investigation shines a beacon of hope for patients who have thus far been excluded from the benefits of conventional treatments. By dissecting the neurobiological roots of treatment resistance through innovative in vivo techniques, it sets a new standard for translational neuroscience and personalized psychiatry.
As the scientific community digests these findings, attention now turns toward developing scalable, accessible neuromodulatory devices and targeted therapeutics that can translate the laboratory advances into tangible clinical outcomes. Ultimately, this research embodies a crucial step toward unraveling the complexity of schizophrenia and improving the lives of millions worldwide.
Subject of Research: Neurophysiological mechanisms underlying treatment-resistant schizophrenia, focusing on GABAergic inhibition and glutamate facilitation.
Article Title: In vivo assessment of GABAergic inhibition and glutamate facilitation in treatment-resistant schizophrenia: a TMS study integrating clinical, cognitive, and neurophysiological evaluations.
Article References:
Barone, A., Senerchia, G., De Simone, G. et al. In vivo assessment of GABAergic inhibition and glutamate facilitation in treatment-resistant schizophrenia: a TMS study integrating clinical, cognitive, and neurophysiological evaluations. Schizophr 11, 90 (2025). https://doi.org/10.1038/s41537-025-00634-w
Image Credits: AI Generated