In a groundbreaking study set to reshape our understanding of colorectal cancer metastasis, researchers have identified a distinct subset of tumor cells that serve as the primary architects of liver metastases. Published recently in Nature Communications, this research dissects the cellular and molecular underpinnings that distinguish these metastatic instigators from their non-metastatic counterparts, shining a transformative light on a persistent oncological enigma: how colorectal cancer spreads to the liver with such lethality and unpredictability.
Colorectal cancer remains one of the leading causes of cancer mortality worldwide, primarily due to its propensity for metastasizing to distant organs, most notably the liver. Despite advances in surgical interventions and systemic therapies, the survival rates for patients with metastatic colorectal cancer remain dismal. This reality underscores a critical urgency for elucidating the mechanisms by which primary colorectal tumors seed distant sites. Alvarez-Villanueva and colleagues ventured into this complex landscape, applying cutting-edge molecular profiling and cellular characterization techniques that have not only mapped but functionally defined a subpopulation of tumor cells bearing hallmarks of metastatic potential.
Central to their discovery is a subpopulation characterized by high expression levels of tight junction proteins and the cell adhesion molecule CDH17 (Cadherin-17). Tight junctions are integral to maintaining epithelial integrity and cell polarity, often disrupted during epithelial-to-mesenchymal transition (EMT), a pivotal process in cancer metastasis. Paradoxically, the research highlights that these metastasis-initiating cells maintain elevated tight junction protein expression, challenging the traditional EMT paradigm that underscores metastatic dissemination as a consequence of junction breakdown and increased cellular motility.
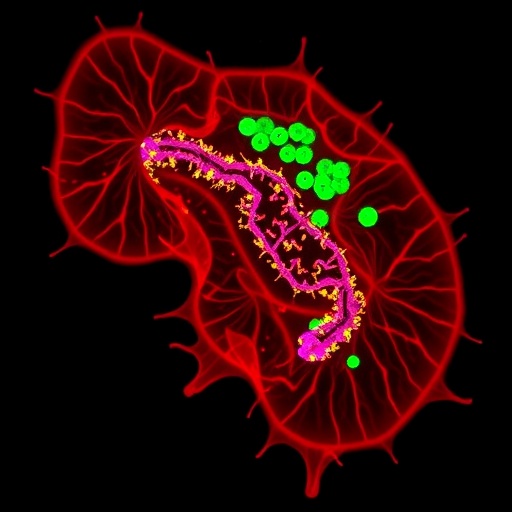
The identification of CDH17 as a marker is particularly novel, given its documented roles in cell-cell adhesion and intestinal epithelial homeostasis. Alvarez-Villanueva’s team demonstrated that CDH17-positive cells within primary colorectal tumors exhibit unique functional properties—enhanced survival, adherence to liver microenvironment constituents, and aggressive colonization capabilities. This population forms a cohesive cluster with maintained intercellular adhesion, suggesting that metastasis may proceed via a collective invasion model rather than by single-cell migration, as previously assumed in many contexts.
Sophisticated in vivo lineage tracing experiments further reinforced these conclusions by showing that liver metastases predominantly originate from this tight junction-high, CDH17-positive population. When selectively ablated or genetically silenced for these markers, the metastatic efficiency was markedly diminished, attesting to their indispensable role in metastatic seeding and outgrowth. This revelation uncovers a potential therapeutic vulnerability, where targeting intercellular adhesion machinery could disrupt metastatic cascade at a fundamental level.
Molecular characterization through single-cell RNA sequencing offered additional insights into the gene expression programs governing these cells. Beyond adhesion molecules, these cells showed enrichment for signaling pathways involved in stemness, survival, and immune evasion, painting a portrait of a highly adapted, resilient tumor cell subtype. Such complexity indicates that these metastasis-initiating cells are not merely phenotypic outliers but possess a multi-faceted biological toolkit optimized for survival in hostile microenvironments.
Intriguingly, the spatial organization of these populations within primary tumors suggested niche-like microenvironments conducive to maintaining their phenotype. The tumor microenvironment, therefore, appears to actively nurture these metastasis-competent cells, opening questions about stromal-tumor interactions and the role of immune components in facilitating metastatic priming.
This research also challenges therapeutic dogma by implicating junctional complexes—traditionally viewed as tumor suppressive—as potential facilitators of malignancy in specific contexts. The clinical implications are profound: treatments aimed indiscriminately at disrupting tight junction integrity might inadvertently promote metastatic dissemination. Clinical trials involving agents targeting adhesion must carefully consider these nuances.
Moreover, the research opens avenues for developing diagnostic biomarkers with prognostic value. Detection of elevated CDH17 and tight junction protein levels in primary colorectal tumors could serve as predictive indicators for liver metastasis risk, enhancing patient stratification and tailoring surveillance protocols accordingly.
From a translational perspective, this discovery prompts renewed enthusiasm for novel drug development focused on modulating cell adhesion molecules or their downstream effectors. Antibodies, small molecules, or even CRISPR-based gene editing techniques might be harnessed to selectively inhibit the metastatic subset without compromising normal tissue integrity.
Furthermore, this study adds to the growing body of evidence that cancer metastasis is a highly regulated process dependent on cellular subpopulations with distinct phenotypic and molecular traits rather than random dissemination. Such refined understanding elevates the conceptual framework guiding research in oncology, moving toward more sophisticated models that incorporate cellular hierarchies and interactive tumor ecosystems.
These groundbreaking insights contribute to a broader narrative emphasizing the need to dissect tumor heterogeneity not only at the genetic but also at the functional and spatial levels. The integration of multi-omics datasets with advanced imaging and in vivo models positions research at a cusp of discovery, where targeted interventions might finally stem the lethal tide of metastatic colorectal cancer.
As the oncology community digests these findings, the hope is that clinical translation follows swiftly. Personalized medicine approaches could integrate these molecular markers into clinical workflows, refining therapeutic strategies to intercept metastasis before it manifests clinically.
Future research directions, as the study suggests, include exploring the interaction dynamics between CDH17-positive cell populations and the hepatic microenvironment, the immune landscape modulation during metastatic colonization, and the potential plasticity of these cells under therapeutic pressure.
In sum, Alvarez-Villanueva et al.’s study breaks new ground by pinpointing a clearly defined, adhesion-rich cellular source driving colorectal liver metastases. Challenging existing assumptions about EMT and metastasis, their work invites a paradigm shift in how scientists and clinicians approach one of oncology’s toughest challenges, promising a future where metastatic disease might be anticipated, intercepted, and ultimately conquered through targeted molecular intervention.
Subject of Research: Cellular mechanisms and molecular identity of colorectal cancer cells responsible for liver metastases.
Article Title: Tight junction-high and CDH17-positive cell population is the source of colorectal cancer liver metastases.
Article References:
Alvarez-Villanueva, D., Maqueda, M., Harti, D. et al. Tight junction-high and CDH17-positive cell population is the source of colorectal cancer liver metastases. Nat Commun (2026). https://doi.org/10.1038/s41467-025-68169-3
Image Credits: AI Generated