In a groundbreaking new study published in Translational Psychiatry, researchers have delved deep into the enigmatic workings of the human brain, focusing on how trauma exposure shapes the intricate connections within the thalamus. Utilizing ultra-high-field 7 Tesla resting-state functional MRI (fMRI), this research provides unprecedented insight into whether the brain’s thalamic subdivisions act as a hub of resilience or as markers of vulnerability in individuals who have experienced trauma. The findings not only illuminate the subtle neural underpinnings of psychological adaptation but also hold promise for refining therapeutic approaches tailored for trauma-exposed populations.
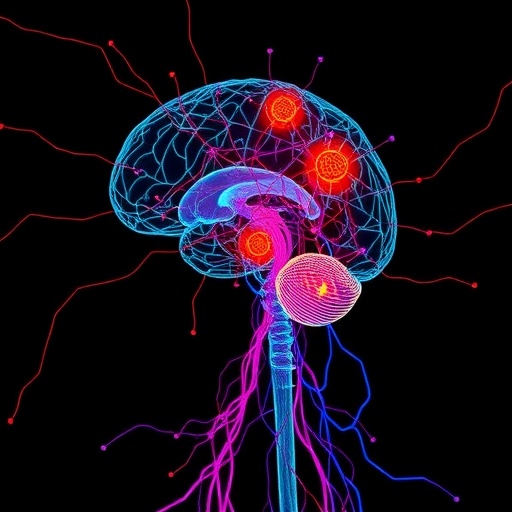
The thalamus, a central brain region traditionally recognized as a relay station for sensory and motor signals to the cerebral cortex, has emerged as a critical player in emotional regulation and cognitive processing, especially under conditions of stress. This study capitalizes on advancements in neuroimaging technology that allow scientists to map minute connectivity patterns within thalamic subdivisions—an endeavor that was previously inhibited by the spatial resolution limits of conventional MRI scanners. Deploying the 7 Tesla resting-state fMRI technique, the authors were able to capture intricate functional connectivity profiles that distinguish between thalamic regions implicated in either resilience mechanisms or susceptibility to trauma-related psychopathology.
One of the pivotal challenges in neuropsychiatric research has been disentangling the neural correlates that distinguish resilient individuals — those who maintain mental health after trauma — from those who develop disorders such as PTSD or depression. This new research leverages the granularity of 7T fMRI to analyze resting-state networks across distinct thalamic nuclei. The team observed that variations in connectivity strength and network integration within these nuclei correlate strongly with individual differences in trauma outcomes, suggesting that the thalamus is not a uniform entity but rather a mosaic of functionally specialized modules influencing coping trajectories.
Specifically, the findings reveal that increased connectivity between certain thalamic subdivisions and prefrontal cortical regions tends to be a hallmark of resilience. This enhanced thalamocortical coupling likely facilitates adaptive regulation of emotional processing and executive function, enabling trauma-exposed individuals to buffer stressful experiences more effectively. In contrast, reduced connectivity or dysregulated network patterns in alternate thalamic subdivisions appear linked to heightened vulnerability, potentially underpinning symptoms such as hyperarousal, intrusive memories, and impaired cognitive control seen in trauma-related psychiatric disorders.
The methodological rigor of the study stands out, especially through the use of resting-state paradigms which eliminate task-related confounds and capture intrinsic brain activity dynamics. Such an approach enables a purer investigation of baseline connectivity states that could serve as biomarkers for predicting individual resilience or risk profiles. It also broadens our understanding of how intrinsic network properties sculpt neurobehavioral outcomes post-trauma, a concept that may revolutionize early identification of those at risk.
Furthermore, the authors underscore the importance of the thalamus’s subdivision-specific roles rather than treating it as a monolithic structure. For example, connectivity patterns involving the mediodorsal nucleus are implicated in higher-order cognitive functions and emotional regulation, whereas the pulvinar nucleus relates more to visual attention and sensory integration. These nuanced insights pave the way for targeted interventions that could selectively modulate dysfunctional circuits, employing neuromodulation or precision pharmacotherapy tailored to discrete thalamic pathways.
Beyond clinical implications, this research also raises profound questions about the neuroplastic capacity of the human brain in the aftermath of trauma. The adaptive connectivity changes observed in resilient individuals hint at the dynamic nature of neural circuits, capable of rewiring in response to environmental pressures. Such plasticity may be harnessed therapeutically to bolster recovery and mental well-being, potentially shifting the paradigm from symptom management to proactive resilience enhancement.
The technology itself — 7 Tesla fMRI — heralds a new era in brain imaging. By offering exceptional signal-to-noise ratios and spatial resolution, it permits visualization of submillimeter-scale brain structures and fine-grained connectivity details previously inaccessible. This breakthrough enables researchers not only to parse thalamic subdivisions but also to explore other brain regions involved in trauma and stress-related processes with unprecedented clarity.
Notably, the integrative analysis combining imaging data with clinical assessments enriches the interpretability of results. Participants underwent thorough psychological profiling, allowing correlations to be drawn between altered connectivity patterns and behavioral manifestations of trauma response. This fusion of neuroimaging and psychometrics embodies the future of personalized psychiatry, where multimodal data converge to inform diagnosis and treatment.
The study also paves the way for larger longitudinal investigations to track how thalamic connectivity evolves over time and in response to therapeutic interventions. Understanding temporal dynamics could offer vital clues about critical windows for intervention when neural circuits are most malleable. Such insights could revolutionize post-trauma care by informing timing, modality, and intensity of treatments.
In essence, this pioneering research eloquently articulates the dualistic nature of the thalamic network’s response to trauma — acting either as a pillar of resilience through enhanced connectivity or as a signature of vulnerability marked by dysregulated circuitries. It exemplifies how sophisticated neuroimaging combined with robust clinical frameworks can unravel the complex brain-behavior relationships underpinning mental health resilience, opening avenues for transformative clinical applications.
As mental health awareness continues to ascend globally, studies like this underscore the critical need to understand the brain’s biological response to trauma beyond symptom-centered diagnostics. They highlight the intricate neurobiological architecture shaping individual destiny in the face of adversity, offering hope that science may soon deliver tailored strategies for fostering resilience at the neural level.
Ultimately, the implications extend far beyond trauma research, illuminating fundamental principles of brain organization, connectivity, and plasticity that resonate across disciplines from cognitive neuroscience to psychiatric therapeutics. The thalamus, long overshadowed by cortical regions, takes center stage as a dynamic hub whose connectivity patterns may hold the key to unlocking human resilience and vulnerability alike.
Such innovative endeavors hold the promise of reshaping our conceptual frameworks and clinical paradigms, inspiring a future where neurotechnology not only deciphers but also heals the fractured human mind, ushering in a new dawn of precision mental health care.
Subject of Research:
Thalamic subdivision connectivity in trauma-exposed individuals and its relationship to resilience and vulnerability, explored using 7T resting-state fMRI.
Article Title:
“Resilience or vulnerability? Thalamic subdivision connectivity in trauma-exposed individuals: a 7 t resting-state fMRI study.”
Article References:
Khudeish, N., Ravichandran, R., Sawalma, A.S. et al. Resilience or vulnerability? thalamic subdivision connectivity in trauma-exposed individuals: a 7 t resting-state fMRI study. Transl Psychiatry (2025). https://doi.org/10.1038/s41398-025-03774-w
Image Credits: AI Generated