In an era where healthcare delivery is increasingly pivoting towards virtual platforms, a recent study sheds critical light on how telehealth has transformed the management of hypertension among adults in the United States. Titled “Use of Telehealth and Antihypertensive Medications Among US Adults with Hypertension,” the research, led by experts Liu and Chaitoff, provides a comprehensive examination of the intersection between telehealth and the administration of antihypertensive medications. This study, published in the Journal of General Internal Medicine, emerges at a critical juncture, as the healthcare system adapts to the challenges posed by the COVID-19 pandemic and beyond.
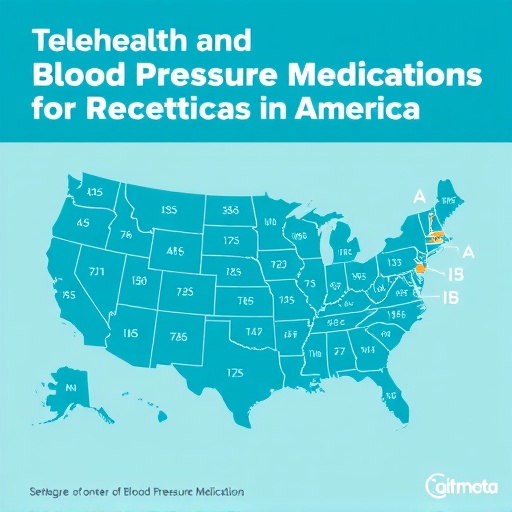
Hypertension, commonly known as high blood pressure, affects millions of Americans and is a major risk factor for cardiovascular disease and stroke. The Centers for Disease Control and Prevention (CDC) estimates that nearly half of U.S. adults have hypertension, making it imperative to find effective management strategies. Telehealth has emerged as a promising tool to bridge gaps in care, especially for patients who may struggle to access traditional in-person appointments. The study highlights the extent to which telehealth has been adopted to monitor and manage hypertension, offering insights into its effectiveness and utilization metrics.
Before delving into the findings, it is essential to understand the utilization patterns of telehealth in relation to antihypertensive medications. The study notes a marked increase in telehealth consultations among patients diagnosed with hypertension, especially during periods when social distancing measures were in effect. This shift towards virtual healthcare has not only enabled patients to receive timely medical advice but also provided ongoing monitoring of their condition without the need for physical visits. As healthcare systems continue to evolve, the implications of these findings could shape future hypertension management protocols.
One of the salient points raised in the study is the demographic shifts in telehealth utilization. The research indicates that while telehealth reached broader patient populations, certain groups—such as those from lower socioeconomic backgrounds—remain at a disadvantage. This digital divide raises significant concerns about health equity, a vital issue in the context of hypertension management. By analyzing patient demographics and their corresponding uptake of telehealth services, the study emphasizes the necessity for targeted interventions aimed at improving access for vulnerable populations.
Moreover, the study delves into the relationship between telehealth usage and adherence to antihypertensive medications. Preliminary findings suggest that patients engaged through telehealth platforms exhibited higher medication adherence rates compared to their counterparts who relied solely on traditional office visits. The robust follow-up and adherence behavior may be attributed to the convenience and accessibility of telehealth services, wherein patients are more likely to discuss medication side effects or adjustment needs during virtual consultations.
In exploring the effectiveness of telehealth in hypertension management, the study also highlights the varying degrees of patient satisfaction. While many patients report a favorable experience with telehealth services, concerns linger about the necessity of in-person examinations for comprehensive care. Patients often question the thoroughness of virtual check-ups, particularly for conditions that require physical assessments or laboratory tests. The need to balance virtual and in-person visits is underscored, leading to discussions about hybrid models of care that could enhance patient outcomes.
Furthermore, the study reviews the technological barriers that may impede the effective use of telehealth. Issues such as internet access, technological literacy, and digital device availability can disproportionately affect certain demographics. There’s a pressing need for healthcare providers and policymakers to recognize these barriers and implement strategies that ameliorate access to telehealth, thus facilitating better hypertension management across diverse populations.
The implications of this study extend beyond hypertension alone. The successful integration of telehealth services in managing chronic conditions could serve as a blueprint for other areas of healthcare. By analyzing the impact of telehealth on medication adherence and patient engagement, the research lays the groundwork for broader applications in chronic disease management.
As telehealth continues to evolve, ongoing research is crucial to understand its long-term viability in managing chronic diseases like hypertension. Future studies should focus on refining telehealth methodologies and exploring their impact over extended periods. This is essential not only to gauge effectiveness but also to establish best practices for virtual healthcare.
Additionally, integration with electronic health records (EHR) can enhance the efficiency of telehealth consultations for hypertension management. By allowing seamless communication between patients and providers, EHR systems can ensure that health data is available in real-time, thus facilitating better decision-making and care coordination.
Patient education and engagement strategies are vital components highlighted in the study. Providing patients with educational resources about hypertension, its management, and the role of telehealth can empower them to take charge of their health. This proactive approach promotes greater awareness of medication adherence and encourages patients to actively participate in their treatment plans.
In conclusion, the study underscores the transformative potential of telehealth in the management of hypertension among U.S. adults. As healthcare continues to embrace digital innovations, the lessons learned from this research can guide future practices, policies, and research aimed at optimizing hypertension care. With a focus on equitable access and patient-centered care, the findings may reshape the narrative of chronic disease management in an increasingly digital world.
The trend towards telehealth signifies a pivotal shift in how healthcare is delivered, promising a more efficient and accessible approach to chronic disease management. As we look ahead, harnessing the power of technology while maintaining the essential human element of healthcare will be key to improving outcomes for patients grappling with hypertension and beyond.
Subject of Research: Telehealth and antihypertensive medications use among US adults with hypertension.
Article Title: Use of Telehealth and Antihypertensive Medications Among US Adults with Hypertension
Article References:
Liu, T., Chaitoff, A., Bress, A. et al. Use of Telehealth and Antihypertensive Medications Among US Adults with Hypertension.
J GEN INTERN MED (2025). https://doi.org/10.1007/s11606-025-09731-z
Image Credits: AI Generated
DOI: 10.1007/s11606-025-09731-z
Keywords: Telehealth, Hypertension, Antihypertensive medications, Patient adherence, Health equity, Chronic disease management.