In an unprecedented exploration of immunological pathways related to myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS), researchers have unveiled critical findings that promise to reshape our understanding of this enigmatic condition. Myalgic encephalomyelitis, often mischaracterized or poorly understood, carries with it debilitating symptoms that affect millions of people worldwide. The new study sheds light on how abnormal T-cell activation and variations in cytotoxic T-cell frequencies may correlate with the severity of symptoms experienced by patients.
T-cells are a pivotal component of the body’s immune defense system, responsible for identifying and neutralizing pathogens. Their role in chronic illnesses like ME/CFS has long been debated, as researchers grapple with understanding the underlying mechanisms that contribute to sustained fatigue and cognitive dysfunction. The latest research simplifies this complex interplay between the immune system and the spectrum of symptoms experienced by those affected by ME/CFS.
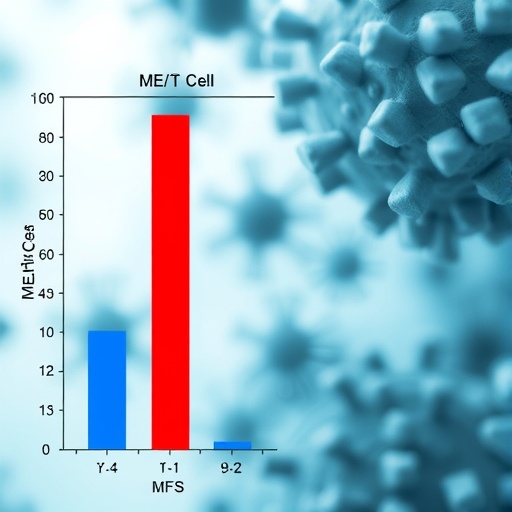
By analyzing blood samples from a variety of patients diagnosed with ME/CFS, the research team, led by Lee, JS., along with collaborators Lacerda and Kingdon, concentrated on identifying specific T-cell markers that could signify heightened immune response. What they discovered was striking: there was a distinct link between the levels of cytotoxic T-cells and the severity of fatigue and other associated symptoms. This finding suggests that an overactive immune response might be a driving factor for many patients suffering from this chronic condition.
The study meticulously categorized the patients based on symptom severity, enabling researchers to assess whether the immune response varied significantly among those at different ends of the spectrum. Notably, participants exhibiting more severe symptoms showed noticeably increased T-cell activation compared to those with milder manifestations. This correlation reinforces the hypothesis that the immune system plays a crucial role in the pathogenesis of ME/CFS, a fact that has significant implications for potential therapeutic interventions.
Furthermore, the intricacies of T-cell dysfunction revealed in the data capture the duality of the immune system’s role. While the body’s natural response to pathogens is critical for health, excessive or misplaced activation can lead to tissue damage and chronically systemic fatigue. The adverse effects extend beyond mere physical exhaustion; cognitive functions and emotional well-being are also impacted, leading to a reduced quality of life for patients. As the research elucidates the mechanisms at play, pathways for treatment may begin to emerge, prioritizing immune modulation strategies.
The implications of these findings are profound, especially considering that ME/CFS is currently inadequately addressed by conventional medicine. Traditional treatment options have focused primarily on symptom management rather than addressing underlying biological factors. With the new insight into T-cell dynamics, the study calls for increased focus on immune-targeted therapies that can potentially alter the trajectory of the disease for patients suffering from its most debilitating forms.
Importantly, progression in understanding ME/CFS is hindered by the stigma surrounding the condition. Often dismissed or misrepresented in both medical literature and popular media, many patients feel compelled to fight for recognition and adequate care. The findings from this research can serve as a beacon of hope, validating the experiences of countless individuals who have long suffered without clear answers. A rigorous scientific approach to understanding the immune system’s involvement in ME/CFS could lead to more compassionate and effective healthcare solutions.
The data derived from this study reinforce the notion that ME/CFS is not a psychological ailment, as it has often been perceived. The biological evidence points toward significant immunological dysregulation, pushing healthcare professionals to reconsider their approaches to diagnosis and treatment. These revelations could prompt new research into early diagnostic markers and intervention strategies that prioritize the biological realities of the condition rather than relying solely on subjective symptom reporting.
In light of these findings, the medical community faces a critical junction. They must balance the pursuit of new therapies with the imperative to educate about ME/CFS. Without awareness and recognition of the complexities surrounding this disease, many patients may continue to navigate their journeys toward healing without support. Efforts in public health to disseminate factual information about ME/CFS and its implications need to become a priority to foster understanding and legislative movement towards better care.
As this research continues to resonate within the medical community, it stands as a clarion call for further investigations into the various components of immune dysregulation. The study lays a foundation for future research that could explore how lifestyle factors, environmental triggers, and genetic predispositions play into the immunological landscape of ME/CFS. Researchers now have the opportunity to delve deeper into the nuances of immune function, exploring potential therapeutic avenues that could alleviate the burden of this complex illness.
The journey to understanding ME/CFS is ongoing, but this research signifies a crucial step forward. As we expand our knowledge on immune response and symptom severity, it becomes imperative for both medical professionals and researchers to advocate for patients. Recognizing the significance of the findings is essential not only for scientific progress but also for the lives of individuals living with ME/CFS who seek answers and relief.
The bright light of scientific discovery shines on a path previously shrouded in confusion and suspicion. The correlation between abnormal T-cell activation and symptom severity may offer invaluable insights for the future of ME/CFS treatment protocols. As we look ahead, it is clear that a more nuanced understanding of the immune system could radically alter the landscape of patient care and recovery strategies tailored for ME/CFS.
By meticulously unpacking the immune dysfunction present in ME/CFS patients, researchers have opened the door to a deeper inquiry into the condition’s etiology. This essential work beckons the next generation of scientists and practitioners to harness this newfound knowledge. With continued focus and collaboration, we can hope to translate these findings into impactful treatment regimens that empower patients reclaim their lives from the grip of chronic fatigue.
In conclusion, the exploration of abnormal T-cell activation and its link to symptom severity is a critical milestone in our understanding of ME/CFS. As research continues to unfold, there is a growing optimism that it could herald a new era in therapeutic approaches. For many, this study holds more than statistical significance; it embodies a glimmer of hope for validation, recognition, and ultimately, better health outcomes in the realm of chronic fatigue syndrome.
Subject of Research: T-cell activation in myalgic encephalomyelitis/chronic fatigue syndrome
Article Title: Abnormal T-Cell activation and cytotoxic T-Cell frequency discriminate symptom severity in myalgic encephalomyelitis/chronic fatigue syndrome
Article References:
Lee, JS., Lacerda, E., Kingdon, C. et al. Abnormal T-Cell activation and cytotoxic T-Cell frequency discriminate symptom severity in myalgic encephalomyelitis/chronic fatigue syndrome. J Transl Med (2025). https://doi.org/10.1186/s12967-025-07507-x
Image Credits: AI Generated
DOI: 10.1186/s12967-025-07507-x
Keywords: myalgic encephalomyelitis, chronic fatigue syndrome, T-cell activation, immune dysfunction, symptom severity