In a groundbreaking advance that could revolutionize the treatment landscape for ovarian cancer, researchers have unveiled compelling evidence that the Tβ4–17 peptide significantly enhances the chemo-sensitivity of ovarian cancer cells to cisplatin (DDP), a widely used chemotherapeutic agent. This discovery, rooted in meticulous molecular biology and oncology research, highlights the peptide’s ability to modulate the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) signaling pathway, a critical regulator of cancer progression and chemoresistance. As ovarian cancer remains one of the deadliest gynecological malignancies worldwide, with resistance to chemotherapy posing a formidable challenge, this novel peptide presents a beacon of hope for improving patient outcomes.
The study illuminates the intricate mechanisms by which Tβ4–17 peptide intervenes in the cancer cell signaling milieu, curbing the survival advantages that ovarian cancer cells often exploit. NF-κB signaling pathway is notorious for its role in promoting inflammation, cell proliferation, and survival—factors that bolster chemoresistance across various cancer types, including ovarian carcinoma. By attenuating NF-κB activation, the Tβ4–17 peptide effectively dismantles the protective shield cancer cells deploy against cisplatin-induced apoptosis, thereby restoring the cells’ vulnerability to the chemotherapeutic agent’s cytotoxic effects.
Ovarian cancer’s prognosis has been historically grim, primarily due to its late clinical presentation and rapid development of resistance to platinum-based chemotherapy. Cisplatin, or DDP, despite its initial efficacy, often fails as cancer cells adapt and evade death signals through complex molecular pathways. The NF-κB pathway, frequently activated in ovarian cancer, promotes tumor survival and metastasis, orchestrating a network of genetic and epigenetic changes that culminate in reduced treatment response. Thus, targeting this pathway has emerged as a strategic imperative in oncology research, and Tβ4–17 peptide’s modulatory influence on NF-κB marks a pivotal breakthrough.
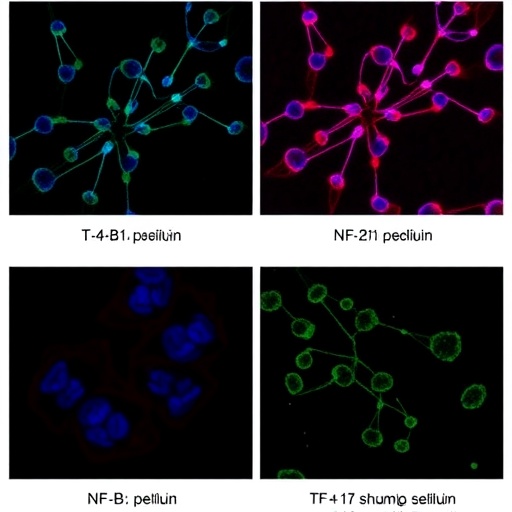
Investigations conducted through a series of in vitro experiments elucidated that Tβ4–17 peptide treatment leads to a reduction in NF-κB transcriptional activity. This downregulation correlates with diminished expression of downstream anti-apoptotic genes, leading to enhanced apoptotic cell death upon cisplatin administration. The synergy between Tβ4–17 and DDP was observed in multiple ovarian cancer cell lines, suggesting a broad therapeutic potential rather than a cell line-specific phenomenon. Importantly, the peptide alone exhibited minimal cytotoxicity, underscoring its role as a sensitizer rather than a standalone cytotoxic agent.
Delving deeper into the molecular crosstalk, the research delineated that Tβ4–17 disrupts the phosphorylation and subsequent nuclear translocation of NF-κB subunits, mainly p65, a critical step for NF-κB’s transcriptional activity. This interference prevents the activation of gene networks responsible for evading apoptosis and fostering drug resistance. These findings not only clarify the mechanistic underpinnings of the peptide’s action but also position it as a precision tool in modulating intricate oncogenic signaling.
The ramifications of these insights extend beyond the laboratory. With chemotherapy resistance being a cornerstone of poor prognosis in ovarian cancer, integrating Tβ4–17 peptide into therapeutic regimens could potentiate cisplatin efficacy, reduce the necessary dosage, and thereby mitigate the notorious side effects associated with high-dose chemotherapy. This combinatorial approach might increase the therapeutic window, offering a dual benefit of amplified anti-cancer efficacy and enhanced patient quality of life.
Furthermore, the study hints at the potential of Tβ4–17 to abrogate other pro-survival pathways intersecting with NF-κB signaling, such as the PI3K/Akt and MAPK cascades. While the precise interactions remain to be comprehensively mapped, the peptide’s ability to influence a central signaling hub imparts it with the versatility to counteract multifaceted resistance mechanisms that ovarian cancer cells employ. This multi-targeted impact imbues Tβ4–17 with substantial promise as a next-generation adjuvant therapy.
Translational implications are profound, as this discovery paves the way for clinical trials aimed at evaluating the safety, optimal dosing, and therapeutic efficacy of Tβ4–17 peptide in combination with cisplatin in ovarian cancer patients. The anticipation is that through rigorous phase I and II clinical investigations, this peptide could transition from bench to bedside, ultimately altering the current clinical paradigm. Moreover, its application could extend to other malignancies wherein NF-κB-driven chemoresistance is prevalent, broadening the scope of its impact.
The cancer biology community has lauded this study’s robust experimental design, combining molecular assays, cell viability assessments, apoptosis quantification, and signaling pathway analyses. Such comprehensive scrutiny ensures that the observed chemo-sensitization effect is reliable and reproducible, setting a high standard for future research exploring peptide-based therapeutic modulators. The inclusion of diverse ovarian cancer subtypes enhances the generalizability of the findings, increasing confidence in the peptide’s clinical applicability.
In addition to its direct therapeutic potential, the Tβ4–17 peptide represents a model for how small peptides can be engineered or harnessed to modulate intracellular signaling networks with high specificity and efficacy. This knowledge propels the field towards a renaissance of peptide therapeutics in oncology, a domain previously constrained by delivery and stability challenges. Advances in peptide engineering and nanoparticle-based delivery systems will likely accelerate the clinical translation of such molecules.
The intersection of molecular oncology and peptide therapeutics encapsulated in this study also spotlights the need for personalized medicine approaches. Given the heterogeneity of ovarian tumors, predictive biomarkers assessing NF-κB activity or peptide responsiveness will be invaluable in identifying patients most likely to benefit from Tβ4–17 adjunct therapy. Future research directions may thus incorporate precision diagnostics alongside therapeutic innovation.
Moreover, the implications for overcoming multidrug resistance (MDR), frequently mediated by NF-κB-induced expression of efflux pumps and survival proteins, are immense. Tβ4–17’s inhibitory effect on NF-κB may downregulate these resistance factors, reinstating sensitivity not only to cisplatin but potentially to other chemotherapeutic agents. This broad-spectrum re-sensitization would be a game changer in combating refractory ovarian cancer.
An exciting prospect arises from the peptide’s minimal direct cytotoxicity, indicating that its clinical tolerability is likely favorable. By enhancing chemo-sensitivity rather than exerting independent toxicity, Tβ4–17 may avoid common off-target effects, a crucial advantage in oncology drug development. This feature also supports combination regimens, which increasingly dominate modern cancer therapy.
The research also paves the way for investigations into the peptide’s pharmacokinetics and pharmacodynamics in vivo. Understanding its stability, distribution, metabolism, and clearance will be vital for optimizing therapeutic protocols. Preclinical animal models are the logical next step, with studies expected to verify efficacy and safety in systemic administrations and tumor microenvironment contexts.
As clinicians and scientists strive to push beyond the limitations of current chemotherapies, the discovery of Tβ4–17 peptide’s chemo-sensitizing properties through NF-κB pathway modulation represents a significant stride. It embodies a targeted, molecularly informed approach to dismantling ovarian cancer’s defenses and heralds a new chapter in how we might win the fight against this aggressive malignancy.
In conclusion, the integration of Tβ4–17 peptide into ovarian cancer treatment paradigms holds immense promise for transforming standard-of-care interventions. By strategically impairing NF-κB signaling to restore chemosensitivity, this approach not only refines therapeutic efficacy but also offers hope for improved survival and quality of life among patients. The impending challenge lies in translating these pioneering findings through clinical pipelines to make a tangible impact in oncology practice.
Subject of Research: The enhancement of cisplatin chemo-sensitivity in ovarian cancer cells mediated through modulation of the NF-κB signaling pathway by the Tβ4–17 peptide.
Article Title: Tβ4–17 peptide enhances the chemo-sensitivity of ovarian cancer cells to DDP by affecting NF-κB signaling pathway.
Article References:
Guo, L., Wang, H., Li, N. et al. Tβ4–17 peptide enhances the chemo-sensitivity of ovarian cancer cells to DDP by affecting NF-κB signaling pathway. Med Oncol 42, 541 (2025). https://doi.org/10.1007/s12032-025-03106-4
Image Credits: AI Generated