In the rapidly evolving field of psychiatric neuroscience, a groundbreaking study has emerged, shedding new light on the intrinsic brain dynamics that underlie bipolar disorder in youth. This research provides unprecedented insights into the longitudinal stability of mood-related resting-state networks in adolescents and young adults diagnosed with symptomatic bipolar-I and bipolar-II disorders. By leveraging advanced neuroimaging techniques alongside sophisticated analytical approaches, the investigation transcends prior cross-sectional snapshots, revealing how these brain networks maintain consistent patterns over extended periods despite the episodic nature of mood fluctuations characteristic of bipolar illness.
Central to this study is the exploration of resting-state functional connectivity — a method that examines spontaneous brain activity when individuals are not engaged in explicit tasks. Resting-state paradigms have gained immense traction due to their ability to capture the brain’s default mode and intrinsic organization. In patients with mood disorders, disturbances in resting-state networks have been frequently reported, yet their stability and evolution over time in youth remain poorly understood. Here, the authors ambitiously track the same individuals across multiple time points to determine whether the neural substrates of mood dysregulation manifest enduring alterations or if they fluctuate in parallel with symptomatic states.
The research cohort comprises young participants diagnosed with bipolar-I or bipolar-II disorder, conditions marked by alternating episodes of mania or hypomania and depression, often with a complex clinical course. By focusing on symptomatic youths — rather than individuals in remission — the study targets the neural signature corresponding directly to mood instability, thus enhancing ecological validity. Longitudinal monitoring over months or years enabled the differentiation of trait-related neural alterations from transient state-dependent changes, a distinction critical for biomarker development and therapeutic targeting.
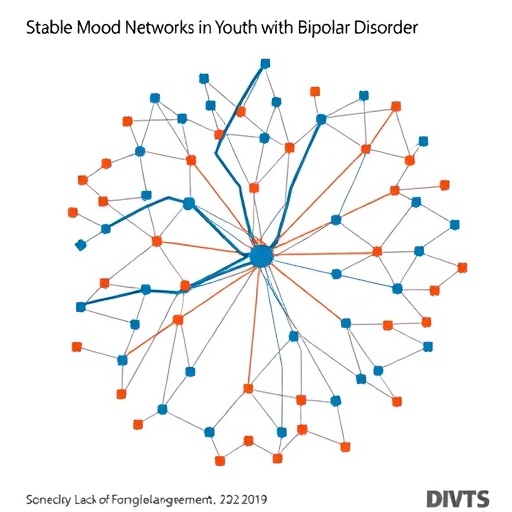
Employing functional magnetic resonance imaging (fMRI) as the primary data acquisition modality, the investigators meticulously assessed brain connectivity within canonical mood-related networks, including the default mode network (DMN), salience network (SN), and limbic circuits. Collectively, these systems orchestrate emotional regulation, attention, and reward processing—domains profoundly disrupted in bipolar disorder. The analytical framework incorporated network-based statistics and graph-theoretical models, allowing quantification of network topology, efficiency, and modularity with remarkable precision.
One of the pivotal findings was the demonstration of high test-retest reliability in key mood-related resting-state networks, suggesting that certain aberrations in connectivity are not merely epiphenomena of mood episodes but may represent stable neurobiological traits. Such traits could serve as enduring markers for diagnosis or risk stratification, potentially guiding personalized interventions. Intriguingly, some connectivity measures exhibited subtle modulation corresponding with clinical mood changes, highlighting the dynamic interplay between enduring network architecture and symptomatic expression.
The implications of these observations extend far beyond theoretical neuroscience. Clinically, bipolar disorder in youth poses significant challenges due to diagnostic complexity, heterogeneity, and the risk of poor long-term outcomes when treatment initiation is delayed. Objective neural markers that remain consistent over time could drastically enhance early diagnosis, monitor treatment response, and ultimately improve prognosis. This study’s longitudinal design underscores the feasibility and necessity of integrating repeated neuroimaging assessments in clinical research and practice.
Moreover, the investigation addresses a critical gap in psychiatric research: the underrepresentation of adolescent and young adult populations in longitudinal neuroimaging studies. Most prior research has focused on adult bipolar cohorts, where brain plasticity and illness trajectories differ markedly. By targeting youth with active symptoms, this study captures a developmental window pivotal for intervention, as brain networks are still maturing and may be more amenable to modulation.
Technical execution of the study reflects cutting-edge neurobiological research standards. Rigorous preprocessing steps controlled for potential confounds such as head motion, scanner drift, and physiological noise, thereby enhancing data integrity. Furthermore, the inclusion of multi-echo fMRI sequences improved signal-to-noise ratios, allowing detection of subtle changes within the resting-state networks. Statistical power was bolstered by including a sufficiently large sample and multiple scanning sessions, facilitating robust longitudinal inferences.
The study also explored correlations between network stability and clinical variables, such as symptom severity, medication status, and functional outcomes, although these analyses revealed complex relationships. For instance, certain disruptive patterns in connectivity were linked with greater mood lability and impaired psychosocial functioning, suggesting a neurobiological substrate for clinical heterogeneity. Nevertheless, pharmacological effects could not be entirely disentangled, underscoring the need for further research into medication influences on neural dynamics.
Significantly, these findings contribute to an expanding conceptual framework that views bipolar disorder not simply as an episodic illness but as a disorder with linked persistent network disruptions. This perspective aligns with emerging models of psychiatric conditions as network-based dysfunctions rather than isolated regional abnormalities. Understanding the stability of these neural networks may pave the way for neuromodulatory therapies, such as transcranial magnetic stimulation or neurofeedback, tailored to restore healthy connectivity patterns.
Looking ahead, the authors advocate for extending this line of inquiry by incorporating multimodal imaging techniques, such as diffusion tensor imaging (DTI) to map white matter integrity and electroencephalography (EEG) to capture rapid electrophysiological changes. Multidimensional datasets could unravel mechanistic pathways bridging structural and functional neural alterations in bipolar youth. Additionally, integrating genetic and environmental data may elucidate factors modulating network stability, enabling precision psychiatry.
In sum, this pioneering research advances the neurobiological understanding of bipolar disorder’s developmental trajectory by affirming that key mood-related brain networks demonstrate remarkable longitudinal stability in symptomatic youth. This challenges prevailing assumptions about transient neural disruptions during mood episodes and highlights the potential for trait-like brain network markers to transform clinical practice. The marriage of rigorous longitudinal fMRI methodology with a developmentally focused cohort sets a new standard for future investigations aiming to decode the complex neural fabric of mood disorders.
As bipolar disorder continues to impose significant public health burdens, particularly among young populations navigating critical life transitions, studies like this illuminate pathways toward improved diagnosis and intervention. Through the integration of neuroscience, psychiatry, and data science, the quest to decode mood-related brain networks offers hope for nuanced, biology-informed treatments that can mitigate suffering and foster resilience in youth.
The continuing exploration of resting-state connectivity dynamics exemplifies the power of neuroimaging to capture the brain’s spontaneous functional organization, which remains a frontier in psychiatric research. By anchoring future work on these foundational findings, the field moves closer to unraveling the intricacies of brain network stability and its disruption in major mood disorders. Such knowledge holds promise for ushering in an era of brain-guided precision psychiatry, tailored not only to diagnosis but also to individualized pathways of recovery.
As scientific inquiry refines our understanding of bipolar disorder’s neural underpinnings, collaborative cross-disciplinary efforts will be essential to translate these insights from bench to bedside. Harnessing longitudinal neural metrics may ultimately revolutionize therapeutic paradigms, offering young patients personalized strategies to sustain mood stability and live fulfilling lives.
Subject of Research: Longitudinal stability of mood-related resting-state brain networks in youth with symptomatic bipolar-I/II disorder.
Article Title: Longitudinal stability of mood-related resting-state networks in youth with symptomatic bipolar-I/II disorder.
Article References: Hafeman, D.M., Feldman, J., Mak, J. et al. Longitudinal stability of mood-related resting-state networks in youth with symptomatic bipolar-I/II disorder. Transl Psychiatry 15, 187 (2025). https://doi.org/10.1038/s41398-025-03404-5
Image Credits: AI Generated