In a groundbreaking advancement in cancer research, scientists have unveiled the pivotal role of KMT2A silencing in orchestrating apoptosis and cell cycle arrest within high-grade serous ovarian carcinoma (HGSOC) cells. This revelation sheds new light on the molecular intricacies of tumor suppression and offers a promising therapeutic avenue that capitalizes on the modulation of gain-of-function (GOF) p53-dependent pathways. As ovarian cancer remains one of the deadliest gynecological malignancies worldwide, this discovery marks a significant milestone in the ongoing quest for more effective treatments.
The crux of this research pivots on the enzyme KMT2A, also known as mixed-lineage leukemia 1 (MLL1), a histone methyltransferase responsible for catalyzing the methylation of lysine 4 on histone H3 (H3K4). This epigenetic modification plays a crucial role in chromatin remodeling and gene expression regulation, influencing oncogenic pathways. Dysregulation of KMT2A has been implicated in various malignancies, but its specific influence on HGSOC and its interaction with mutant p53 proteins had remained elusive until now.
Mutations in the TP53 gene, which encodes the tumor suppressor protein p53, are a hallmark of HGSOC. Intriguingly, many of these mutations confer a gain-of-function phenotype upon the p53 protein, diverging from its canonical role and instead facilitating oncogenesis by activating aberrant transcriptional programs. This dual nature complicates therapeutic targeting, as GOF mutant p53 not only loses tumor suppressor activity but actively promotes cancer progression. The interplay between KMT2A and mutant p53 proteins thus emerges as a critical axis in tumor cell survival and proliferation.
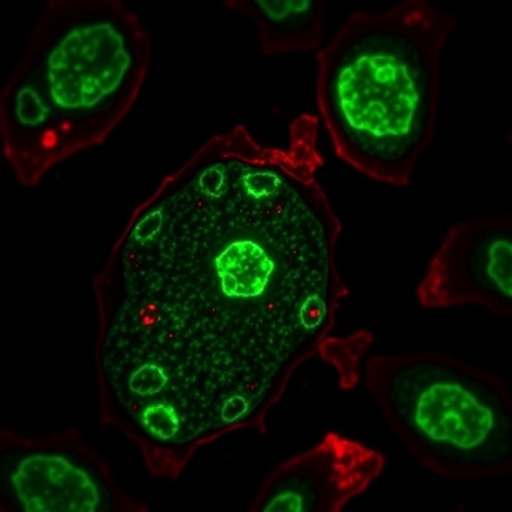
Researchers employed small interfering RNA (siRNA) to selectively silence KMT2A expression in established HGSOC cell lines. This targeted knockdown led to significant induction of programmed cell death, known as apoptosis, and disrupted the normal progression of the cell cycle, effectively halting cellular replication. Mechanistically, this effect was traced back to alterations in gene expression profiles governed by the mutant p53, underscoring the dependency of HGSOC cells on the KMT2A-driven epigenetic landscape for maintaining their malignant phenotype.
Detailed analyses revealed that KMT2A silencing diminished the transcriptional activity of genes commonly upregulated by GOF mutant p53. This shift created a hostile environment for tumor cell viability, as pro-survival and proliferative pathways were suppressed. Concurrently, genes that promote apoptotic cascades and cell cycle checkpoints were upregulated, tipping the balance in favor of tumor suppression. This dual regulatory role highlights the sophisticated epigenetic control exerted by KMT2A within the oncogenic milieu.
The implications of this study extend beyond the immediate molecular mechanisms. Targeting the epigenetic modifiers in cancer cells represents a burgeoning frontier in precision oncology, especially as current therapies for HGSOC often encounter resistance and relapse. KMT2A emerges as a viable drug target, offering opportunities to disrupt the malignant circuitry maintained by mutant p53 proteins. This could pave the way for combination therapies that integrate epigenetic modulators with standard chemotherapeutic agents, potentially enhancing efficacy and overcoming treatment-resistant disease.
Importantly, the research underscores the necessity of stratifying patients based on their TP53 mutational status and KMT2A expression levels. Personalized medicine approaches could leverage this novel biomarker axis to identify those who stand to benefit most from KMT2A-targeted interventions. The advent of siRNA-based therapeutics and emerging delivery platforms bolster the translational potential of these findings, bringing benchside insights closer to clinical applicability.
The study also elucidates the broader epigenomic landscape reshaped by KMT2A activity. Chromatin immunoprecipitation sequencing (ChIP-seq) assays demonstrated that KMT2A occupies critical promoters and enhancers modulated by mutant p53. This co-localization facilitates aberrant transcriptional activation essential for tumor maintenance. Disruption of this interface via KMT2A knockdown effectively dismantles the oncogenic transcriptional hubs, further validating the target’s centrality in tumor biology.
Beyond ovarian cancer, the functional nexus between KMT2A and GOF mutant p53 may have wider oncological relevance. Mutant p53 variants are prevalent across a spectrum of solid tumors, suggesting that epigenetic modulation of this pathway could be a generalized therapeutic strategy. Future studies are warranted to explore the applicability of KMT2A silencing in other p53-mutant malignancies, potentially broadening the impact of these findings.
The utilization of siRNA technology itself is emblematic of the precision medicine era. By harnessing molecular specificity to silence oncogenic drivers at the RNA level, researchers can minimize off-target effects and toxicity commonly associated with conventional drugs. The fine-tuning of delivery mechanisms and chemical modifications to enhance siRNA stability are essential ongoing endeavors that will determine the clinical success of such therapies.
Moreover, the intersection of epigenetics and mutant p53 biology as revealed by this study signifies an evolution in understanding tumor pathophysiology. Epigenetic regulators like KMT2A do not merely modulate gene expression in isolation but interact dynamically with mutant p53 to sculpt the cancer transcriptome. This synergistic model redefines therapeutic targeting paradigms and underscores the complexity of cancer’s regulatory networks.
In summation, the strategic inhibition of KMT2A unveils a compelling vulnerability in the otherwise refractory landscape of high-grade serous ovarian carcinoma. By triggering apoptosis and arresting the cell cycle through modulation of gain-of-function p53-dependent pathways, this approach disrupts the malignant equilibrium and proposes a refined pathway for intervention. As researchers refine these molecular tools and translate them into clinical trials, hope surges for patients grappling with this formidable disease.
This discovery not only enriches the fundamental understanding of HGSOC’s molecular underpinnings but also aligns with the broader movement toward targeted epigenetic therapies. As oncology strides into an era defined by molecular precision and adaptive therapeutics, KMT2A stands out as a beacon of hope—a molecular switch that can be flipped to halt cancer in its tracks. The scientific community eagerly anticipates subsequent phases of research to validate and expand upon these transformative findings.
With continuing advances in genomics, proteomics, and drug delivery, the horizon for KMT2A-directed therapies appears increasingly attainable. The fusion of cutting-edge biotechnology with clinical oncology promises to reshape therapeutic landscapes, transforming ovarian cancer from a fatal diagnosis into a manageable condition. This innovative approach, rooted in dissecting the molecular symbiosis between epigenetic enzymes and mutant tumor suppressors, exemplifies the future of cancer care—intelligent, targeted, and efficacious.
The challenge now lies in bridging the gap between laboratory insights and real-world clinical applications. Multidisciplinary collaborations involving molecular biologists, pharmacologists, and oncologists will be instrumental in navigating this transition. Moreover, patient-derived models and sophisticated in vivo systems will be crucial to rigorously test safety and efficacy profiles before clinical rollout. The journey from discovery to bedside demands perseverance, but with the stakes this high, every stride forward holds transformative potential.
In conclusion, the silencing of KMT2A unveils a novel, mechanistically grounded therapeutic avenue for combating high-grade serous ovarian carcinoma. By modulating gain-of-function p53-dependent pathways, it induces cell death and halts tumor progression, addressing a critical need in current oncological treatment paradigms. This landmark study paves the way for innovative epigenetic strategies that could redefine ovarian cancer management and provide renewed hope to patients worldwide.
Subject of Research: Therapeutic targeting of KMT2A in high-grade serous ovarian carcinoma through modulation of gain-of-function mutant p53 pathways
Article Title: (Not provided)
Article References: (Not provided)
Image Credits: AI Generated
DOI: (Not provided)
Keywords: KMT2A, siRNA, apoptosis, cell cycle arrest, high-grade serous ovarian carcinoma, gain-of-function p53, epigenetics, tumor suppression, targeted therapy