In a groundbreaking new study published in 2026, researchers have unveiled compelling evidence indicating that risperidone, a widely prescribed antipsychotic medication, can significantly reduce morphometric similarity deviations in the brains of individuals diagnosed with schizophrenia. This discovery not only sheds light on the neurobiological underpinnings of schizophrenia but also bridges a novel link between the drug’s effects and distinct cortical transcriptomic patterns, opening new avenues for precision psychiatry and therapeutic interventions.
Schizophrenia, a complex and multifaceted psychiatric disorder characterized by hallucinations, delusions, cognitive impairments, and emotional dysregulation, has long challenged neuroscientists and clinicians alike. Despite its prevalence, affecting approximately 1% of the global population, the precise neural alterations underlying schizophrenia remain incompletely understood. Morphometric similarity, a neuroimaging metric that quantifies structural similarity across brain regions, has emerged as a powerful tool to evaluate brain network integrity and aberrations in neuropsychiatric conditions. Deviations in morphometric similarity reflect atypical cortical organization which is thought to underpin dysfunctional brain connectivity observed in schizophrenia patients.
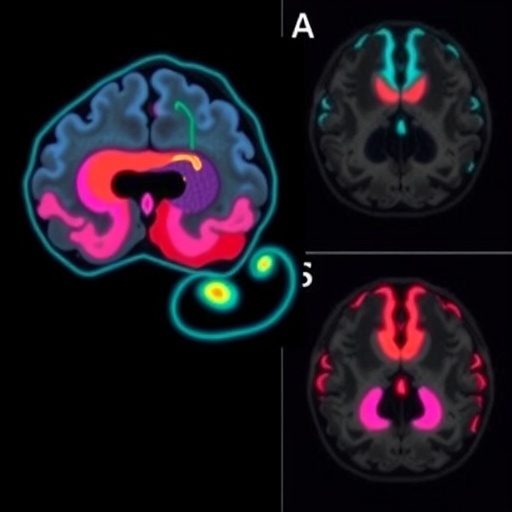
The new study, led by Liu, Yang, Chen, and their collaborators, employed state-of-the-art neuroimaging techniques combined with individualized morphometric analyses to assess the extent to which risperidone modulates these structural abnormalities. Through longitudinal MRI assessments, the researchers tracked alterations in cortical morphometric similarity metrics before and after risperidone treatment in schizophrenia cohorts, revealing a marked normalization effect. Crucially, the extent of reduction in morphometric similarity deviation correlated with improvements in clinical symptomatology, highlighting the therapeutic relevance of these neural changes.
What truly sets this research apart is its integrative multi-omics approach. Beyond imaging, the team incorporated cortical transcriptomic data—essentially gene expression profiles from affected brain regions—to probe molecular mechanisms potentially driving morphometric alterations and their remediation with risperidone. Their analysis identified distinct gene expression patterns linked to synaptic plasticity, neurotransmitter pathways, and neuroinflammatory processes, which appear intricately tied to the morphometric reorganization observed in patients post-treatment.
This convergence of morphometric and transcriptomic evidence suggests risperidone’s action extends beyond symptomatic relief and touches fundamental biological substrates, including modulation of gene networks associated with cortical structure and function. Understanding how psychopharmacological agents recalibrate these gene expression profiles offers unprecedented insight into molecular pathways exploitable for next-generation therapeutics targeting schizophrenia’s core pathology.
Moreover, the concept of individualized morphometric similarity deviation advances the precision medicine paradigm within psychiatry. Treatment responses can be idiosyncratic, and the ability to quantify patient-specific brain network deviations provides a quantitative biomarker to track disease progression and tailor interventions accordingly. This methodology heralds a move away from broad-spectrum antipsychotic use towards more refined, mechanism-based strategies aligned with each patient’s unique neuroanatomy and molecular signature.
The broader implications of these findings resonate deeply within neuroscience and clinical psychiatry. They validate morphometric similarity deviation as a critical biomarker for schizophrenia, endorse risperidone’s neural reparative properties, and illuminate transcriptomic landscapes that could serve as drug targets. Future trials integrating these biomarkers may optimize dosing protocols and predict response trajectories more accurately, reducing trial-and-error prescribing and enhancing patient outcomes.
This research also invigorates ongoing discussions about the neurodevelopmental versus neurodegenerative nature of schizophrenia. The reversible normalization of morphometric abnormalities post-risperidone administration suggests plasticity within affected circuits, countering notions of irreversible brain deterioration and supporting rehabilitative therapeutic approaches. It invites reexamination of schizophrenia’s clinical staging, urging clinicians to intervene early to harness this neuroplastic potential.
Furthermore, the identification of transcriptomic alterations associated with treatment response broadens our understanding of schizophrenia as a disorder deeply rooted in gene-environment interactions. It lays groundwork for combining pharmacotherapy with epigenetic or gene expression-modulating interventions in the future, potentially enabling synergistic effects that improve long-term functional recovery.
The technological tools implemented in this study—high-resolution MRI, advanced neuroanatomical mapping, and integrative transcriptomics—highlight the increasing sophistication of contemporary psychiatric research. Their successful application exemplifies the power of interdisciplinary methodologies to unravel psychiatric illness complexities, a trend expected to drive the field forward in coming years.
Importantly, this work underscores the need for continued research into antipsychotic mechanisms at multiple biological scales, from synaptic physiology to systemic brain network dynamics. Such multilevel understanding is critical to design drugs with enhanced specificity and fewer side effects, given that current antipsychotics often carry substantial adverse burdens impacting patient adherence and quality of life.
In sum, the findings by Liu, Yang, Chen, et al. provide a compelling narrative about the neural substrates modulated by risperidone in schizophrenia, combining morphometric neuroimaging and molecular neuroscience to offer a holistic view of treatment effects. This integrative approach exemplifies the future of psychiatric research, where clinical, imaging, and genomic data converge to optimize diagnosis, monitoring, and therapeutics. As science marches toward unraveling the enigma of schizophrenia, studies such as this inch us closer to truly personalized medicine—a hope long cherished but only now becoming achievable.
Ultimately, these advances highlight that despite schizophrenia’s complexity, targeted interventions can recalibrate dysfunctional brain architecture and associated molecular abnormalities. Such discoveries renew optimism for patients and caregivers, reinforcing the potential of science to transform devastating mental illnesses from chronic burdens into manageable conditions with tangible recovery prospects. As further investigations build on this foundation, the prospect of precision psychiatry grounded in neuroimaging and cortical transcriptomics will reshape clinical paradigms and improve countless lives worldwide.
Subject of Research: The effect of risperidone on morphometric similarity deviation in schizophrenia and its association with cortical transcriptomic patterns.
Article Title: Risperidone reduces individualized morphometric similarity deviation in schizophrenia and associates with cortical transcriptomic patterns.
Article References: Liu, L., Yang, M., Chen, J. et al. Risperidone reduces individualized morphometric similarity deviation in schizophrenia and associates with cortical transcriptomic patterns. Schizophr (2026). https://doi.org/10.1038/s41537-025-00724-9
Image Credits: AI Generated