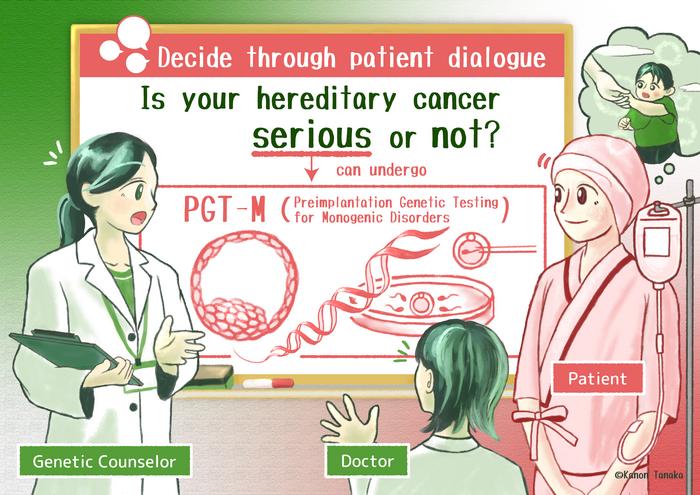
A groundbreaking study led by a team of Japanese researchers has critically revisited the criteria used to evaluate the “seriousness” of genetic conditions, with a focus on hereditary cancers and their implications for preimplantation genetic testing (PGT). Conducted in Hiroshima in early 2025, the research highlights the transformative role that patient experiences and stakeholder voices play in reshaping medical and ethical frameworks traditionally grounded in narrow clinical parameters. Published in the European Journal of Human Genetics in March 2025, this correspondence offers pivotal insights into balancing clinical assessments with lived realities, a conversation of growing significance amid rapid advances in genetic diagnostics and reproductive technologies.
Genetic disorders have long been assessed using rigid medical criteria that prioritize quantifiable clinical severity. In Japan, this approach remains entrenched, leading to restrictive policies governing access to PGT for monogenic disorders. Currently, the Japanese Society of Obstetrics and Gynecology permits PGT for only seventeen conditions, reflecting a conservative framework that often excludes a broader understanding of disease impact. However, cases such as retinoblastoma—which surged into recognition as a “serious” disorder only after persistent patient advocacy spanning six years—exemplify the limitations of strictly clinical categorizations and underscore an urgent need to integrate patient and stakeholder perspectives into these evaluations.
Central to this inquiry was the adoption of a conceptual framework proposed by Kleiderman and colleagues, which dissects the notion of “seriousness” into multidimensional core components and procedural elements. This advanced understanding acknowledges not only medical criteria but also factors such as treatment accessibility, support resources, and crucially, individual and familial lived experiences. The framework offers a comprehensive lens through which Japanese stakeholders—patients, healthcare professionals, and ethicists—could reevaluate their perceptions during a two-stage survey conducted at a stakeholder dialogue event in Hiroshima.
The study’s methodology entailed an initial phase where participants were provided with detailed clinical information regarding the medical thresholds for preimplantation genetic testing eligibility, treatment modalities, and available support systems. This foundational exposure centered discussions around objective medical data and the infrastructures supporting affected individuals. Subsequently, the session featured poignant testimonies from patients living with hereditary cancers, including genetic profiles marked by retinoblastoma and BRCA2 mutations. This juxtaposition of empirical facts with personal narratives invited participants to engage deeply with the human dimension of genetic disorders often obscured in clinical dialogue.
Before exposure to patient stories, a significant majority—66% of survey participants—expressed readiness to consider preimplantation genetic testing if confronted with hereditary cancer in their familial lineage. This initial stance reflected a common preventative desire to avert the transmission of debilitating genetic conditions. Moreover, an overwhelming 89% advocated for informing patients about PGT options at diagnosis, revealing a robust consensus on the ethical imperative for transparency and patient education within clinical settings.
Remarkably, these initial perceptions evolved after the participants absorbed firsthand accounts of living with hereditary cancer. There was a statistically significant decline in the perception of PGT as merely a public health instrument aimed at reducing societal burden, indicated by a p-value of 0.005. Instead, greater emphasis emerged on individual reproductive autonomy, underscoring personal choice and agency in genetic decision-making. Favorable attitudes toward marriage, pregnancy, and family planning in the context of PGT rose markedly from 54% to 71%, evidencing how patient voices can recalibrate ethical considerations and reshape communal understandings of what constitutes “seriousness” in genetic disease.
The shift in perspective highlighted by this study emphasizes that lived experiences are not ancillary but central to resilient ethical frameworks guiding genetic testing policies. Put simply, the human, emotional, and psychosocial realities of those affected must weigh alongside clinical data when defining eligibility for advanced genetic interventions. Dr. Rie Iizuka of Hiroshima University articulated this transformative insight, stressing the need to transcend reductive medical models in favor of more nuanced and inclusive policy designs that respect reproductive autonomy and the diverse ways families experience genetic illnesses.
Despite its novel contributions, the research team cautions against overgeneralization due to certain limitations. The participant cohort was relatively small and comprised individuals who were already engaged in PGT-related discourse, possibly introducing selection biases that could skew results. Additionally, the study’s scope was confined to hereditary cancer stakeholders, thereby excluding voices from other genetic conditions whose experiences might further broaden the ethical and clinical landscape. These limitations highlight the imperative for subsequent studies to incorporate larger, more varied populations both nationally and internationally.
Looking ahead, the researchers aim to expand this inquiry, adopting a more inclusive recruitment approach that embraces diverse genetic disorders and a wider demographic spectrum. The ultimate goal is to provide robust empirical validation for Kleiderman et al.’s proposition that assessments of genetic condition seriousness must evolve beyond clinical metrics to genuinely incorporate stakeholder lived experiences. Such integration promises to refine guidelines that govern preimplantation genetic testing, ensuring they are attuned to ethical subtleties and real-world complexities faced by patients and families.
The study also operates as a critique of global genetic testing paradigms, where countries vary significantly in policy transparency and criteria for PGT access. While many nations have broadened their scope to include a wider array of monogenic disorders, Japan remains comparatively restrictive, revealing the cultural, legal, and ethical dynamics unique to each healthcare landscape. By illuminating how ethical frameworks can evolve through participatory stakeholder engagement, this research offers a potential model for international dialogues on the governance of genetic reproductive technologies.
Embedded within this discourse is the tension between public health objectives and respecting individual autonomy. Traditionally, genetics and reproductive policies in many societies have navigated this balance cautiously, wary of implications ranging from social stigma to eugenics concerns. The Japanese case exemplifies how deep engagement with patient narratives can pivot stakeholders toward prioritizing autonomy, challenging policies that have long emphasized societal burden reduction as a primary justification for restricting genetic interventions.
These findings carry profound implications for clinical geneticists, bioethicists, policy-makers, and patient advocacy groups. They mandate a reevaluation of communication strategies around PGT, emphasizing the ethical necessity of comprehensive patient education that incorporates not only medical facts but also relatable lived experiences. Clinics and policy bodies may need to reconsider consent processes, eligibility criteria, and support frameworks to align them with this emerging paradigm that honors the complexity of genetic disease beyond its molecular descriptors.
The research team, comprising Shizuko Takahashi, Rie Iizuka, and Tsutomu Sawai, collectively hailing from prestigious institutions including Hiroshima University and the National University of Singapore, exemplifies interdisciplinary collaboration bridging bioethics, genetics, and clinical practice. Their work benefits from funding by the Japan Society for the Promotion of Science KAKENHI, the JST Research Institute of Science and Technology for Society, and the Uehiro Foundation on Ethics and Education, reflecting robust support for advancing ethical engagement with cutting-edge genetic science.
As genetic technologies surge ahead, this study serves as a timely reminder that ethical progress lags if patient voices remain marginalized. The shift from a predominantly clinical to a deeply experiential understanding of “seriousness” challenges entrenched perspectives and opens pathways for more humane, responsive genetic health policies. The recalibration facilitated by patient testimonies not only redefines seriousness but also champions reproductive freedom and dignity in the genomic era.
Subject of Research: Impact of patient voices on ethical and clinical decision-making in genetic testing for hereditary cancers, focusing on reassessment of “seriousness” in genetic conditions.
Article Title: Reevaluating ‘seriousness’ in genetic conditions: balancing clinical criteria and lived experiences
News Publication Date: 15-Mar-2025
Web References:
- Article: https://www.nature.com/articles/s41431-025-01829-6
- Framework by Kleiderman et al.: https://www.nature.com/articles/s41431-024-01681-0
References:
- Takahashi, S., Iizuka, R., Sawai, T. "Reevaluating ‘seriousness’ in genetic conditions: balancing clinical criteria and lived experiences." European Journal of Human Genetics, 15 March 2025.
Image Credits: Kanon Tanaka
Keywords: Genetic testing, Cancer genetics, Medical ethics, Risk factors