In a groundbreaking retrospective study published in the prestigious journal BMC Cancer, researchers have unveiled critical insights into the prognostic factors influencing survival outcomes in patients with locally advanced cervical cancer (LACC) treated with concurrent chemoradiotherapy (CCRT). This comprehensive investigation sheds new light on the interplay between magnetic resonance imaging (MRI) features, clinical biomarkers, and long-term patient prognosis, guiding future therapeutic decision-making and potentially reshaping clinical management strategies for one of the most challenging gynecologic malignancies.
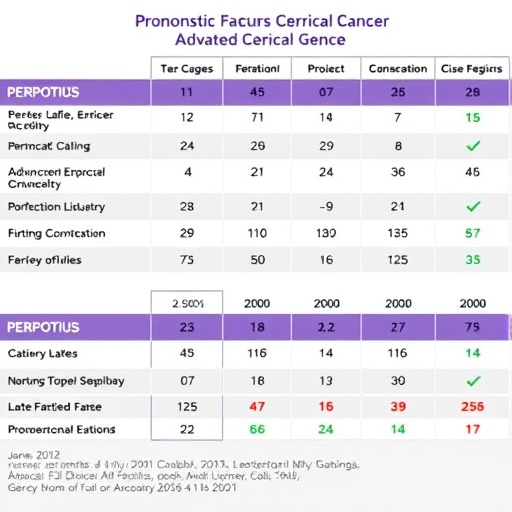
Locally advanced cervical cancer remains a major global health burden, often requiring a combination of chemotherapy and radiotherapy to achieve disease control. Despite advances in treatment modalities, variability in patient outcomes persists, underlying the urgent need for reliable prognostic indicators that can stratify risk and tailor post-treatment surveillance. The study meticulously analyzed data from 189 LACC patients who received definitive CCRT and underwent intensive MRI assessments before and one month after initial therapy, providing an enriched dataset to decode factors correlating with progression-free survival (PFS) and overall survival (OS).
One of the pivotal elements of this research was the evaluation of tumor size and the mean apparent diffusion coefficient (ADC_mean), derived from diffusion-weighted MRI images. These imaging biomarkers have been increasingly explored as non-invasive surrogates reflecting tumor cellularity and microenvironment dynamics. While ADC_mean was hypothesized to serve as a potential predictor of treatment efficacy, the study’s robust multivariate analysis ultimately delineated its limitations, finding that it did not reliably forecast survival outcomes in this cohort. Such findings challenge prevailing assumptions about diffusion-weighted imaging parameters as stand-alone prognostic tools.
Contrastingly, traditional clinical parameters demonstrated significant prognostic relevance. Elevated serum squamous cell carcinoma (SCC) antigen levels, a well-established tumor marker, emerged as a consistent independent predictor for both poorer PFS and OS. This reinforces the role of SCC antigen as a dynamic biomarker reflecting tumor burden and aggressive tumor biology, meriting incorporation into routine post-CCRT monitoring protocols. Clinicians may thus consider more intensive follow-up regimens and adjuvant therapies for patients presenting with high SCC antigen titers.
Furthermore, the study highlighted tumor stage at diagnosis as a formidable determinant of survival probabilities. Patients with advanced-stage tumors were shown to endure markedly worse outcomes, emphasizing the critical importance of early detection and accurate staging in influencing prognosis. Tumor stage remained independently predictive in multivariate models, signifying its enduring value alongside molecular and imaging parameters in comprehensive risk assessment frameworks for LACC.
Another noteworthy revelation concerned the residual disease (RD) size observed one month post-treatment. Residual tumor presence, particularly when measuring equal to or greater than 1.1 centimeters, was strongly correlated with diminished PFS and OS, signifying a resilient tumor cell population refractory to initial chemoradiotherapy. This metric offers a tangible biomarker for clinicians to identify patients at heightened risk of recurrence who may benefit from intensified surveillance or adjunctive interventions aimed at eradicating residual malignancy.
The study also observed that positive pelvic lymph node status was associated with unfavorable outcomes concerning progression-free survival, highlighting the implications of nodal metastasis in disease dissemination and resistance. Moreover, the use of adjuvant chemotherapy following CCRT was paradoxically linked to poorer overall survival, suggesting the need for judicious patient selection and further research into optimizing adjuvant treatment paradigms to avoid overtreatment or adverse effects.
One of the most compelling aspects of this investigation is the extensive median follow-up period of 58 months, an unusually long surveillance window providing valuable longitudinal outcome data. Such mature follow-up allows for robust survival analyses, capturing late recurrences and sustained remission patterns seldom appreciated in shorter-term studies. This strengthens the validity of the prognostic factors identified and their applicability in clinical practice.
From a methodological perspective, the deployment of Cox proportional hazards models alongside univariate and multivariate analyses ensured a rigorous statistical framework to disentangle the independent contributions of various clinical and imaging variables. This robust analytical approach minimized confounding influences and enhanced confidence in the identified prognostic markers, setting a benchmark for future oncologic research designs aimed at survival outcome predictions.
The findings from this study bear important implications for precision oncology in cervical cancer management. Identifying patients with high-risk features such as elevated SCC antigen levels, advanced tumor stage, and significant residual disease affords an opportunity for personalized treatment intensification, tailored follow-up regimens, and early integration of novel therapeutic modalities like immunotherapy or targeted agents currently under investigation.
In addition to clinical utility, these results encourage a paradigm shift in the utilization of MRI biomarkers. The negligible prognostic value of ADC_mean underscores the necessity for integrating multiparametric imaging approaches or combining imaging markers with molecular profiles to develop composite predictive models, enhancing survival predictions and therapeutic planning.
This research also spotlights the critical need for multidisciplinary collaboration involving radiologists, oncologists, pathologists, and biostatisticians to holistically interpret complex datasets derived from advanced imaging, serum markers, and clinical staging. Such integrated efforts are paramount to translating prognostic insights into actionable clinical algorithms that improve patient outcomes.
The comprehensive analysis presented expands the current knowledge landscape regarding locally advanced cervical cancer and reaffirms the enduring relevance of conventional clinical markers alongside modern imaging techniques. By delineating factors that significantly influence progression-free and overall survival, the study equips clinicians with robust evidence to refine prognostication and optimize individualized patient care pathways.
As cervical cancer continues to pose significant therapeutic challenges globally, especially in low-resource settings, these findings may influence screening strategies and resource allocation by identifying key prognostic indicators accessible through routine diagnostic modalities like MRI and serum SCC antigen assays.
Ultimately, this study catalyzes new avenues for clinical research aimed at validating and integrating these prognostic markers into predictive nomograms or decision-support tools, facilitating real-time risk stratification to guide treatment selection and post-therapy surveillance intensity in locally advanced cervical cancer.
With the ongoing advancements in oncologic imaging, molecular diagnostics, and systemic therapies, the pursuit for reliable prognostic determinants remains critical. This landmark investigation not only clarifies which factors hold prognostic weight but also delineates the limitations of current imaging biomarkers, steering future research towards more sophisticated and encompassing prognostic frameworks.
As the oncology community continues to grapple with the complexities of cervical cancer prognosis, the insights garnered from this study provide a foundational step towards enhancing survival outcomes through precision risk assessment and tailored therapeutic approaches, promising hope for improved patient prognoses in the years ahead.
Subject of Research: Prognostic evaluation of MRI and clinical features in patients with locally advanced cervical cancer following concurrent chemoradiotherapy.
Article Title: Prognostic factors of locally advanced cervical cancer after concurrent chemoradiotherapy: a retrospective study
Article References:
Li, X., Mao, Z., Li, Q. et al. Prognostic factors of locally advanced cervical cancer after concurrent chemoradiotherapy: a retrospective study. BMC Cancer 25, 1498 (2025). https://doi.org/10.1186/s12885-025-14691-y
Image Credits: Scienmag.com
DOI: https://doi.org/10.1186/s12885-025-14691-y