In a groundbreaking advance in combating the opioid crisis, Kumar and Butler’s recent study introduces a pioneering machine learning approach to predict opioid overdose deaths across US counties. Their work, published in the International Journal of Mental Health and Addiction, reveals how integrating sophisticated algorithms with explainable artificial intelligence can uncover key risk factors, potentially transforming public health interventions and policy decisions. As the opioid epidemic continues to claim tens of thousands of lives yearly, this new research offers fresh hope for proactive, data-driven strategies that could save lives on a massive scale.
The foundation of the study rests on employing machine learning techniques to analyze extensive datasets covering demographic, socioeconomic, and healthcare-related variables across numerous US counties. By harnessing the power of gradient boosting algorithms, the researchers developed a predictive model capable of identifying counties at elevated risk for opioid overdose fatalities. Unlike traditional epidemiological methods that rely on linear assumptions or limited variables, machine learning models excel in detecting complex, nonlinear interactions within massive datasets. This capability enables more accurate and nuanced predictions that can inform targeted prevention efforts.
Notably, Kumar and Butler placed emphasis on interpretability, employing SHapley Additive exPlanations (SHAP) values to demystify the “black box” nature of their machine learning framework. SHAP values assign importance scores to individual risk factors, elucidating each variable’s contribution to the model’s overdose death risk predictions. This explainability is crucial for translating algorithmic outputs into actionable insights for public health officials and policymakers. It effectively bridges the gap between advanced computational techniques and practical, human-understandable knowledge, fostering trust and enabling precise interventions.
The study’s dataset amalgamated multifaceted county-level information, including health statistics, socioeconomic indicators such as poverty rates and unemployment, demographic profiles, and access to healthcare services. This holistic approach allowed the model to capture the multifactorial nature of the opioid epidemic, recognizing how intertwined community characteristics jointly influence overdose risk. In particular, factors related to social deprivation, healthcare infrastructure, and population demographics emerged as significant predictors, reflecting the epidemic’s roots in systemic socioeconomic disparities rather than isolated individual behaviors.
Training their machine learning model on this vast dataset, Kumar and Butler achieved impressive predictive performance metrics, indicating strong accuracy in distinguishing counties with high versus low opioid overdose death rates. The model’s validation on unseen data strengthened the evidence that such analytics can meaningfully contribute to early warning systems aimed at intercepting overdose trends before they culminate in mortality surges. This predictive power enables more strategic allocation of resources, allowing interventions to be prioritized in communities where they will have maximal impact.
Beyond prediction, the use of SHAP values unveiled critical insights about key risk factors driving opioid overdose deaths. Poverty and unemployment emerged as dominant variables, highlighting the socioeconomic vulnerabilities that exacerbate substance abuse and limit access to treatment. Additionally, the model underscored the role of mental health service availability and opioid prescription rates, providing a nuanced picture of healthcare system influences. By quantifying and ranking these factors, researchers and public health officials gain clarity on which levers to pull for effective overdose prevention.
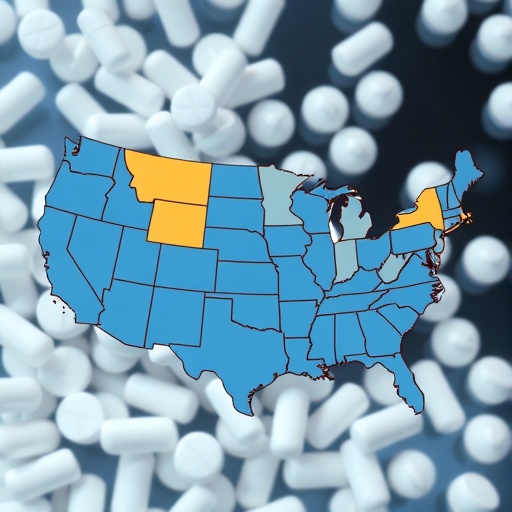
One of the most remarkable aspects of this research lies in its geographic granularity. County-level analysis provides actionable precision, allowing interventions to be tailored to local conditions rather than employing a one-size-fits-all approach at state or national levels. This localized focus respects the heterogeneous nature of the opioid crisis, which varies widely depending on community characteristics such as economic health, social cohesion, and healthcare access. Consequently, the findings foster more equitable and efficient public health strategies.
The machine learning framework’s adaptability also promises utility beyond the initial study scope. Given its modular design, incorporating new data sources or updating models as more recent data becomes available can continually refine and enhance prediction accuracy. This dynamic capability is vital in the fast-evolving landscape of opioid use patterns, where shifts in drug supply, policy changes, and emergency response strategies constantly reshape risk profiles. Future iterations could integrate real-time data streams, such as emergency medical responses or prescription monitoring programs, to further boost responsiveness.
Moreover, the study’s methodological innovations set a precedent for applying explainable AI in other domains of public health surveillance and intervention. By demonstrating how complex models can be rendered interpretable without sacrificing predictive power, Kumar and Butler pave the way for widespread adoption of such tools. Their approach tackles a longstanding barrier: the mistrust and opacity surrounding AI applications in healthcare. As a result, this research contributes to the growing movement toward transparent AI that supports ethical and effective public health decision-making.
The implications for policymakers are profound. Armed with predictive insights and detailed risk factor breakdowns, decision-makers can design more informed and targeted policies addressing root causes of opioid overdose deaths. For example, investments in economic development, mental health services, and healthcare access can be prioritized in counties identified as high risk. Simultaneously, public awareness campaigns and harm reduction initiatives can be fine-tuned to reflect local needs and vulnerabilities. This evidence-based approach promises to optimize the effectiveness of interventions and enhance community resilience.
From a clinical perspective, understanding the socioeconomic and healthcare system-level contributors highlighted by the model may encourage healthcare providers to adopt more holistic approaches to pain management and addiction treatment. Recognizing the interplay between individual patient factors and broader social determinants can guide multidisciplinary care plans that incorporate social services alongside medical treatment. This broader lens is critical in tackling a complex public health crisis that extends far beyond pharmacological interventions alone.
Importantly, the research advocates for integrating data science within public health infrastructure. It underscores the necessity of robust data collection and sharing mechanisms to fuel predictive analytics. Enhanced surveillance capabilities and cross-sector collaborations will be essential to maintain and expand upon the successes demonstrated by Kumar and Butler’s model. Investments in health informatics, data integration, and workforce training in data analytics emerge as key priorities for sustained progress against the opioid epidemic.
The study also highlights ongoing challenges, such as data quality variability and potential biases in machine learning models. The authors acknowledge that while their model performs well, discrepancies in county-level reporting and unmeasured confounders may affect accuracy and generalizability. Addressing these issues will require continuous refinement of data sources and model validation using diverse datasets. Transparency in these limitations is vital for realistic expectations and for guiding future research directions.
In conclusion, Kumar and Butler’s research represents a significant leap forward in the opioid epidemic’s fight by harnessing machine learning and explainable AI to predict overdose deaths and map their drivers at a granular level. Their innovative approach exemplifies the synergy between advanced technology and public health imperatives, opening pathways to smarter interventions and ultimately saving lives. As the ripple effects of this work spread through academic, clinical, and policy circles, it signals a new era where data-driven insights empower communities to confront and conquer one of America’s most daunting health crises.
This pioneering convergence of artificial intelligence and epidemiology offers a hopeful vision of the future—one in which predictive analytics not only forecast tragedy but also illuminate paths toward prevention and recovery. The promise to anticipate opioid overdose outbreaks county-by-county, coupled with transparent explanations of underlying risk factors, equips stakeholders at every level with indispensable tools for making informed, impactful decisions. Kumar and Butler’s contribution marks a critical milestone on this journey, inspiring continued innovation and collaboration to turn the tide on opioid-related deaths across the United States.
Subject of Research: Opioid overdose death prediction and risk factor analysis using machine learning and explainable AI techniques across US counties.
Article Title: Opioid Overdose Death Prediction Using Machine Learning and Risk Factor Analysis Using SHAP Values for US Counties
Article References:
Kumar, V., Butler, R. Opioid Overdose Death Prediction Using Machine Learning and Risk Factor Analysis Using SHAP Values for US Counties. Int J Ment Health Addiction (2025). https://doi.org/10.1007/s11469-025-01563-6
Image Credits: AI Generated