In the relentless quest to conquer glioblastoma, one of the most aggressive and fatal brain cancers, researchers have made a groundbreaking advancement that could redefine personalized cancer therapy. A recent study published in Nature Communications unveils a novel approach centered around the polyclonal expansion of tumor-infiltrating lymphocytes (TILs), harnessing the body’s own immune cells to mount a targeted and multifaceted attack against glioblastoma tumors. This innovative cell therapy strategy may open unprecedented avenues for effective treatment of a malignancy long notorious for its resistance to conventional therapies.
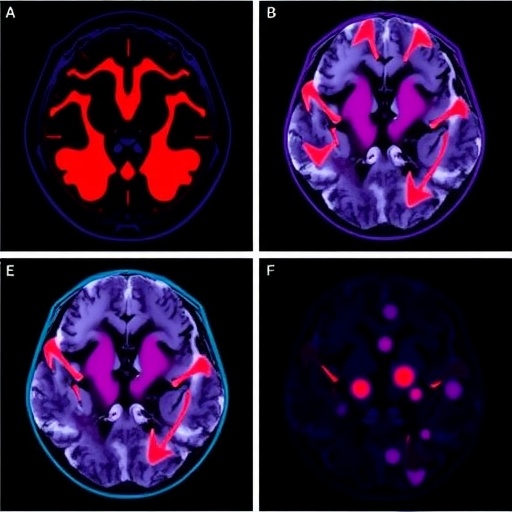
Glioblastoma multiforme (GBM) has presented a formidable challenge in neuro-oncology, primarily due to its highly invasive nature, heterogeneity, and immunosuppressive tumor microenvironment (TME). Previous attempts to employ immunotherapy in GBM have often faltered because the adaptive immune response in the brain is uniquely regulated, and the tumor itself frequently evades immune detection. However, this new research harnesses the polyclonal repertoire of tumor-reactive lymphocytes naturally infiltrating glioblastoma tissues, suggesting a paradigm shift where the immune system’s intrinsic capacity is amplified and redirected for therapeutic benefit.
At the heart of this approach lies the principle of isolating TILs directly from patient tumor samples, followed by their ex vivo polyclonal expansion under conditions that preserve their tumor specificity and effector functions. Unlike monoclonal strategies that rely on single antigen targets and risk immune escape, polyclonal expansion capitalizes on the diverse array of tumor antigens recognized by various T cell clones. This diversity is crucial in GBM, where antigenic heterogeneity and mutational burden complicate targeted therapies.
The study meticulously characterizes the phenotypic and functional attributes of these expanded TIL populations, demonstrating their robust cytotoxic capacity against autologous tumor cells in vitro. Importantly, the investigators employed advanced flow cytometry and single-cell sequencing technologies to elucidate the clonality and transcriptional profiles of the T cells, revealing a rich landscape of tumor-reactive subsets bearing activation markers such as CD137 and PD-1. These features underscore the functional readiness of the TILs for therapeutic deployment.
Moreover, the researchers optimized culture protocols incorporating cytokines like IL-2 and IL-15 to maintain T cell viability and enhance expansion efficiency, balancing proliferation with the retention of a less differentiated, memory-like phenotype. This aspect is critical because terminally differentiated T cells often suffer from exhaustion, limiting their persistence and antitumor efficacy upon infusion. By maintaining the TILs’ proliferative potential and functional fitness, the protocol lays the groundwork for durable therapeutic responses.
Another remarkable facet of this study involves the validation of TIL specificity through functional assays measuring interferon-gamma (IFN-γ) release and cytolysis. The polyclonally expanded lymphocytes exhibited potent tumor cell killing without significant reactivity against nonmalignant brain cells, an essential safety consideration given the delicate neural environment. This tumor-selective cytotoxicity implies that the approach may minimize off-target effects often associated with systemic immunotherapies.
Perhaps most striking is the personalized nature of this cell therapy. Because TILs are harvested directly from each patient’s tumor, the resulting cellular product inherently embodies the unique antigenic landscape of their cancer. This individualized targeting is likely to overcome the heterogeneous mutation profiles that thwart standardized treatments. It also offers a compelling solution to immune evasion mechanisms deployed by glioblastoma, as the broad-spectrum TIL repertoire can adapt to multiple tumor epitopes simultaneously.
The translational potential of this study is underscored by the researchers’ demonstration of in vivo efficacy in orthotopic glioblastoma models. Mice receiving adoptively transferred expanded TILs showed significant tumor regression and prolonged survival compared to controls, providing a proof-of-concept for clinical application. These promising preclinical results pave a path toward human trials, wherein such adoptive cell therapies could be integrated with existing treatment modalities such as surgery, radiotherapy, and checkpoint inhibitors.
This research also sheds light on the intricate interplay between tumor immunology and neurobiology. Understanding how TILs traffic to and survive within the central nervous system, a traditionally immune-privileged site, adds a valuable dimension to immunotherapy design. The ability to expand functional lymphocytes that can overcome the immune barriers imposed by the brain microenvironment is a testament to the evolution of immuno-oncology.
Furthermore, the integration of high-throughput sequencing data with functional assays offers a blueprint for biomarker development. Identifying signatures predictive of TIL expansion success or patient responsiveness will be instrumental in patient stratification and therapy customization. Such biomarkers could inform the selection of candidates most likely to benefit from TIL therapy while sparing others from ineffective treatments.
Despite these advances, challenges remain before this therapy reaches routine clinical use. Manufacturing scalability, regulatory hurdles, and ensuring durable TIL engraftment in patients are critical issues slated for future research. Intratumoral heterogeneity and the potential for immune suppression within glioblastoma also necessitate combination strategies, possibly combining TIL therapy with modulators of the TME or checkpoint blockade to fully unleash antitumor immunity.
Nonetheless, the implications of this research resonate beyond glioblastoma. The methodology for polyclonal TIL expansion and its cross-application to other solid tumors heralds a new era of cell-based immunotherapies that are more adaptable and precise. By leveraging the intrinsic immune repertoire, scientists are edging closer to truly personalized cancer treatments that harness the patient’s own biology rather than relying solely on synthetic drugs.
In summation, the study represents a milestone in neuro-oncology and immunotherapy, providing compelling evidence that functional tumor-reactive lymphocytes can be expanded ex vivo to produce potent, safe, and personalized cell products capable of combating glioblastoma. It captures the essence of next-generation therapies, where immunological nuance and personalized medicine converge to offer hope against a historically intractable cancer.
As the scientific community anticipates clinical trials based on these findings, the growing momentum in adoptive TIL therapy underscores the transformative potential of immunotherapy. This study not only expands our understanding of glioblastoma’s immunobiology but also charts a path forward for innovative treatments that could ultimately improve survival and quality of life for patients facing this devastating diagnosis.
The convergence of immunology, genomics, and cellular engineering exemplified in this research marks a pivotal advancement. By continuing to unravel the complexities of tumor-immune dynamics and refining TIL expansion protocols, precision immunotherapy for glioblastoma may soon transition from promising research to clinical reality, ushering in a new hope for patients worldwide.
Subject of Research: Polyclonal expansion of tumor-reactive lymphocytes infiltrating glioblastoma for personalized cell therapy.
Article Title: Polyclonal expansion of functional tumor-reactive lymphocytes infiltrating glioblastoma for personalized cell therapy.
Article References:
Maffezzini, M., Musio, S., Di Ianni, N. et al. Polyclonal expansion of functional tumor-reactive lymphocytes infiltrating glioblastoma for personalized cell therapy.
Nat Commun 16, 7279 (2025). https://doi.org/10.1038/s41467-025-62263-2
Image Credits: AI Generated