In a groundbreaking advancement in the field of pharmacology and toxicology, researchers have developed a pioneering platform utilizing human liver organoids-on-chip technology to evaluate drug-induced liver injury. With steady increases in drug development failure rates attributed to hepatotoxicity, the call for more predictive preclinical models has never been more pressing. Recent findings spearheaded by Chen et al. underline the critical need for improved methodologies to assess drug safety and efficacy before human trials commence.
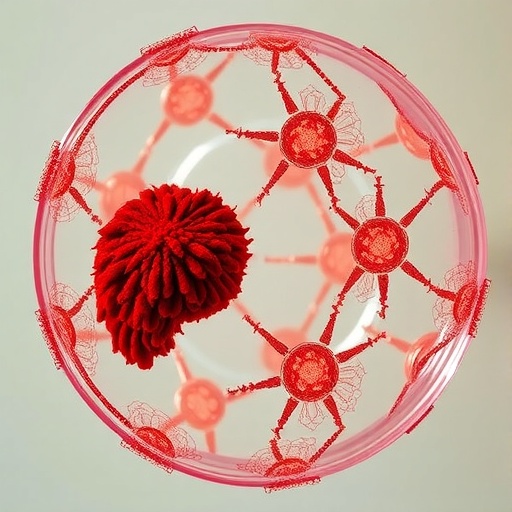
This innovative organoid-on-chip platform emulates the complex architecture and biological functionality of human liver tissues, offering an unprecedented glimpse into drug metabolism and potential toxicological responses. Traditional methods, including animal models, have long faced criticism for their inability to accurately replicate human liver responses. By contrast, this new organoid technology harnesses human stem cells to create miniature liver tissues capable of mimicking the organ’s critical functions while enabling sophisticated drug testing and evaluation.
The construction of human liver organoids involves the intricate derivation of pluripotent stem cells, which are cultivated in 3D environments to spontaneously organize into structures resembling actual liver tissues. This process ensures that the resulting organoids exhibit hepatocyte-like functionality. Such sophisticated construction allows for a more in-depth analysis of metabolic pathways and cellular interactions pivotal in the drug metabolism process while simulating human responses at an unprecedented scale.
One of the pivotal benefits of this liver organoids-on-chip system is its potential to bridge the gap between in vitro studies and clinical drug trials. Researchers have highlighted how existing in vitro platforms often fail to adequately predict human responses owing to the oversimplification of biological systems. The liver organoid system offers a more nuanced understanding of how various drugs could induce cytotoxicity, thereby reducing the dependency on higher-priced and less ethical animal testing.
The platform allows researchers to conduct high-throughput assessments of numerous compounds concurrently, offering efficient analysis and the potential for rapid screening. This approach is notably advantageous when considering the increasing complexity of drug formulations and the expansive array of potential side effects. By employing this organoid-on-chip technology, researchers can significantly accelerate the identification of liver toxicants much earlier in the drug development process.
Notably, the researchers’ study exemplifies the ability of this technology to discern inter-individual variability in drug metabolism and toxicity. Each patient’s liver responds differently to drugs due to genetic factors, pre-existing conditions, and environmental influences. The organoid system allows for the modeling of patient-specific responses, potentially paving the way for personalized medicine approaches in the field of hepatotoxicity assessment.
In their findings, Chen et al. meticulously analyzed how various compounds interacted with the liver organoids, using both high-resolution imaging and biochemical assays to measure drug uptake and toxicity levels. These comprehensive investigations have helped elucidate the biochemical pathways activated during drug metabolism and the resultant cellular stress signaling triggered by hepatotoxic agents. Importantly, the platform has shown promise in distinguishing between compounds that provoke benign effects and those that lead to severe liver damage.
This novel study also raises discussions surrounding the ethical implications of utilizing human-based models over traditional animal testing. With global calls for the replacement, reduction, and refinement of animal models in research, this approach represents a significant stride in ethical research practices. It reflects a growing commitment within the scientific community to prioritize humane methodologies that still generate reliable and valid results.
Moreover, while the implications for pharmaceutical companies are profound, this organoid-on-chip technology also holds promise for regulatory bodies tasked with evaluating drug safety prior to clinical trials. By standardizing toxicological testing protocols and utilizing a human-based model, regulatory agencies can move towards a more scientifically robust and ethically sound evaluation process, reaching decisions quicker and with greater confidence.
Researchers are optimistic that the advent of organoid-on-chip platforms could transform standard practices across drug development pipelines, thereby reducing failure rates and enhancing patient safety. By delivering a more accurate representation of human liver biology, this technology is poised to not only benefit pharmaceutical companies in their drug discovery efforts but also fundamentally reshape the therapeutic landscape in a way that prioritizes patient health.
As evidenced by the outcomes of this study, the organoids-on-chip approach illustrates significant potential in elucidating the molecular mechanisms involved in drug-induced liver injury that were previously obscure. Such discoveries could inform dose adjustments, therapeutic interventions, or even the re-evaluation of existing drugs when unforeseen hepatotoxic effects emerge.
This could ultimately catalyze shifts in both preclinical and clinical methodologies, ensuring that we are no longer relying on rudimentary models for understanding complex human biology. By applying the organoids-on-chip technology, researchers can gain invaluable insights into the evolving relationship between human health, disease, and pharmaceutical interventions.
Moving forward, continued research and development of this organoid technology promise to enhance our comprehension of not only drug-induced liver injuries but also other organ-specific toxicities. As the technology matures, we may witness an explosion of application across other fields of toxicology, which could herald a new age in biomedical research characterized by precision and personalization.
Moreover, as a society grappling with the rising burden of liver diseases, the application of such innovative technological tools may help in devising individualized healthcare strategies that effectively address these challenges. The potential for translating these findings into clinical practice remains a gratifying outcome that researchers and practitioners alike eagerly anticipate.
The implications of this advancement cannot be overstated, as it highlights a pivotal moment in scientific inquiry where ethical considerations converge with technological innovation, ultimately aiming for better health outcomes for the global population. As we broaden our understanding of the toxicological landscape, this organoid-on-chip platform stands out as a beacon of progress, illuminating a path towards a safer and more efficient future in drug development.
Subject of Research: Drug-Induced Liver Injury Assessment Using Human Liver Organoids-on-Chip Technology.
Article Title: A human liver organoids-on-chip for the assessment of drug-induced liver injury.
Article References:
Chen, X., Bao, F., Liu, J. et al. A human liver organoids-on-chip for the assessment of drug-induced liver injury.
BMC Pharmacol Toxicol (2026). https://doi.org/10.1186/s40360-025-01074-z
Image Credits: AI Generated
DOI:
Keywords: organoids-on-chip, drug safety, liver injury, pharmacology, toxicology, stem cells, personalized medicine, ethical research, drug development, preclinical models.