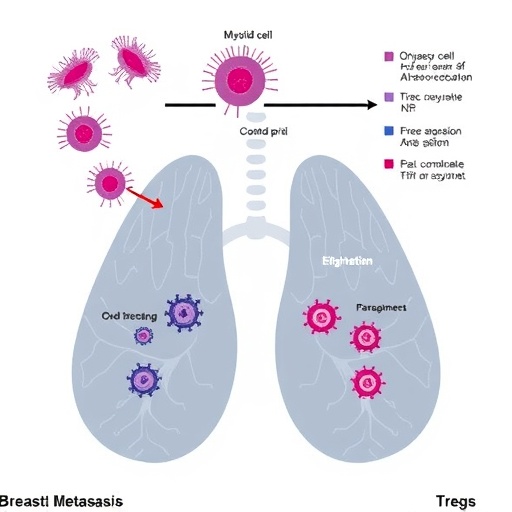
In a significant advancement for breast cancer diagnostics, researchers have uncovered a potent predictive biomarker combination involving myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs), which may transform the approach to identifying lymph node metastasis. This compelling discovery not only deepens our understanding of the immunological landscape in breast cancer but also signals a promising new avenue for improving clinical outcomes through precision medicine.
The study, conducted at the Breast Centre of the Fourth Hospital of Hebei Medical University, meticulously examined peripheral blood samples from 107 breast cancer patients alongside 33 healthy control subjects. By employing sophisticated flow cytometry techniques, the research team quantitatively analyzed the presence and levels of immunosuppressive cellular populations, particularly focusing on the heterogeneity of MDSCs, including polymorphonuclear (PMN-MDSCs) and monocytic (M-MDSCs) subsets, alongside Tregs. These immune cells are notorious for their role in tumor-induced immunosuppression, facilitating cancer progression by subverting the host’s antitumor immune response.
One of the pivotal revelations from this investigation is the marked elevation of MDSCs and Tregs in breast cancer patients relative to healthy individuals. The statistical significance of this increase (p < 0.05) underscores the systemic immunological alterations elicited by malignant processes. Notably, the expansion of these cells is not merely a peripheral phenomenon but intricately linked to the aggressiveness and spread of breast cancer, as evidenced by the robust positive correlation with lymph node metastasis (p < 0.001 for MDSCs, PMN-MDSCs, and Tregs).
Lymph node involvement remains a cardinal prognostic factor in breast cancer, frequently dictating therapeutic strategies and survival outcomes. Conventional methods of detecting metastatic spread involve invasive biopsies or imaging modalities with varying sensitivities. Thus, the identification of reliable blood-based biomarkers that accurately reflect metastatic risk presents an attractive, less invasive clinical tool. The current study’s findings suggest that assessing the combined levels of MDSCs and Tregs in peripheral blood can significantly enhance the predictive accuracy for lymph node metastasis, surpassing the diagnostic value of individual markers.
Receiver operating characteristic (ROC) curve analyses further corroborated these insights. Among the evaluated cell populations, Tregs demonstrated the highest individual area under the curve (AUC = 0.766), affirming their critical role in mediating tumor immune evasion and supporting metastatic dissemination. Importantly, the amalgamation of MDSCs and Treg assessments yielded a combined AUC exceeding that of any single parameter, emphasizing the synergistic potential of these biomarkers when evaluated concomitantly.
Diverging into the biology of these immune suppressive cells, MDSCs represent a heterogeneous group of immature myeloid cells that accumulate in cancer and other pathological conditions, exerting potent immunosuppressive functions primarily through the inhibition of T cell activation and proliferation. Their two principal subsets, PMN-MDSCs and M-MDSCs, differ in morphology, surface markers, and mechanisms of suppression. This study elucidates that both subsets are elevated in breast cancer and significantly associated with metastatic burden, although M-MDSCs portrayed a somewhat weaker yet still relevant association (p = 0.045).
Tregs, characterized by the expression of transcription factor FOXP3, are pivotal regulators of immune homeostasis but often co-opted by tumors to foster a microenvironment conducive to immune tolerance. By curtailing effector T cell responses and secreting immunosuppressive cytokines, Tregs can effectively shield cancer cells from immune surveillance. The current research concretely links heightened peripheral Treg levels with increased lymphatic spread, reinforcing their dual-edged role within the cancer-immune interplay.
Beyond its clinical implications, this study provides mechanistic insights into how the systemic immune milieu shapes tumor evolution and metastasis. The simultaneous elevation of MDSCs and Tregs illustrates a coordinated immunosuppressive network that not only promotes primary tumor development but facilitates dissemination via lymphatics. This paradigm underscores the significance of targeting multiple immune subsets to disrupt metastatic progression effectively.
Furthermore, the ease of measuring these cellular populations through flow cytometry in peripheral blood samples suggests considerable practicality for clinical deployment. Routine monitoring of MDSC and Treg levels could potentially guide risk stratification, inform surgical planning, and tailor adjuvant therapies, ultimately contributing to personalized breast cancer management.
The study also raises intriguing questions for future research, such as the potential for therapies that selectively modulate MDSCs and Tregs to restrain lymph node metastasis. Immunotherapeutic strategies, including checkpoint inhibitors and cell-depleting agents, might be optimized by incorporating biomarker-driven patient selection based on these immune profiles.
From a translational standpoint, the findings emphasize a shift towards integrating immunological biomarkers into conventional oncological workflows. Such integration could expedite early detection of metastatic risk and improve prognostication with minimal patient discomfort compared to existing invasive diagnostics.
Importantly, this research aligns with the broader scientific push to elucidate the tumor microenvironment’s systemic ramifications, recognizing cancer as not merely a localized entity but one profoundly influenced by host immunity. It reaffirms the concept that peripheral immune alterations mirror and potentially dictate tumor behavior.
The robustness of the data, underpinned by a well-characterized patient cohort and rigorous analytical methods, strengthens confidence in these conclusions. However, the authors acknowledge the necessity for larger, multi-center studies to validate these findings across diverse populations and breast cancer subtypes.
In summary, the combined elevation of MDSCs and Tregs emerges as a powerful biomarker axis predicting lymph node metastasis in breast cancer. This discovery portends a new era of immunological diagnostics that harness systemic immune shifts to anticipate metastatic progression, ultimately guiding therapeutic interventions more accurately and improving patient prognoses.
With breast cancer remaining a leading cause of cancer-related morbidity and mortality worldwide, innovations such as this illuminate pathways to earlier intervention and better tailored treatment algorithms. As research continues to unravel the intricacies of tumor-immune dynamics, integrating immune profiling into routine care promises profound impacts on breast cancer management and beyond.
Subject of Research: Investigation of the clinical significance of myeloid-derived suppressor cells (MDSCs), including polymorphonuclear (PMN-MDSCs) and monocytic (M-MDSCs) subsets, and regulatory T cells (Tregs) in peripheral blood of breast cancer patients for predicting lymph node metastasis.
Article Title: Combined elevation of myeloid-derived suppressor cells and Tregs predicts lymph node metastasis in breast cancer.
Article References:
Zhang, H., Yin, X., Wang, S. et al. Combined elevation of myeloid-derived suppressor cells and Tregs predicts lymph node metastasis in breast cancer. BMC Cancer 25, 1806 (2025). https://doi.org/10.1186/s12885-025-15277-4
Image Credits: Scienmag.com
DOI: 10.1186/s12885-025-15277-4 (Published 24 November 2025)