In a groundbreaking new study published in Genus, a leading demographic journal, researchers have unveiled a striking shift in mortality trends across Italy’s regions—a change that could herald the end of a long-standing pattern of regional convergence in life expectancy. This research delves deeply into the complex evolution of mortality rates, shedding light on the multifaceted forces reshaping health outcomes across the Italian peninsula, and raising critical questions about the future of public health policy and regional inequalities.
For decades, mortality rates across Italian regions have exhibited a notable trend towards convergence, as disparities in life expectancy gradually diminished. Traditional socio-economic divides, differing healthcare performances, and regional development disparities had been slowly closing, which lent optimism to policymakers and public health officials. However, the latest analysis by Carboni, Salinari, De Santis, and their collaborators identifies a pronounced reversal or stagnation in this convergence, with some regions experiencing persistent or even worsening mortality outcomes relative to others.
The core of this study is an intricate statistical exploration of mortality data collected over several decades across Italy’s twenty regions. The authors employed advanced demographic modeling techniques to trace and decompose patterns of mortality change, focusing on cause-specific mortality and age-specific mortality trends. This comprehensive approach allowed the researchers to disentangle the influence of various epidemiological and socio-economic factors and to detect subtle shifts masked by aggregate statistics.
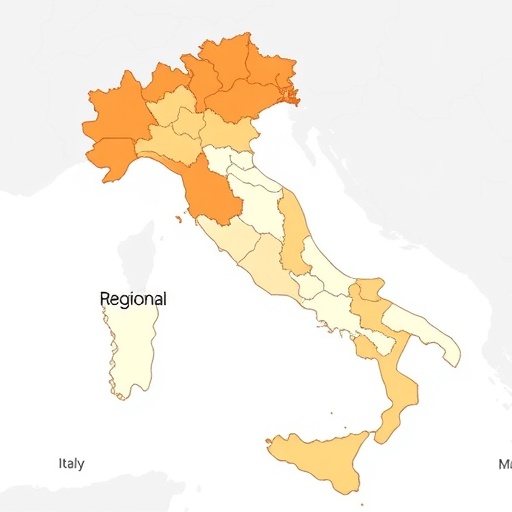
One of the most remarkable facets emerging from the data is the uneven pace of mortality improvement. Northern regions, historically known for higher economic development and better healthcare infrastructure, continue to enjoy incremental gains in life expectancy. Yet in certain southern regions, often characterized by economic disadvantages and limited healthcare accessibility, the pace of improvement has either stalled or reversed for specific age groups and causes of death. This phenomenon disrupts previous assumptions of a steady leveling of life expectancy across Italy.
A particularly important aspect of the analysis lies in the examination of cause-specific mortality. The authors highlight how non-communicable diseases, such as cardiovascular diseases and certain cancers, continue to decline in wealthier regions more rapidly than in economically challenged areas. Meanwhile, causes like respiratory diseases and external causes of death (including accidents and violence) exhibit more erratic trends, sometimes worsening in less advantaged regions. These differences contribute significantly to the persistence of regional mortality variations.
Moreover, the study explores the potential role of health system performance and public health policies in driving these divergent trends. While national healthcare reforms aimed at reducing disparities were implemented over recent decades, their impact may be unevenly distributed due to structural and organizational differences at the regional level. The persistence of healthcare access gaps, variations in preventive care uptake, and disparities in the management of chronic conditions emerge as critical factors influencing mortality evolution.
Lifestyle and behavioral risk factors also feature prominently in the discussion. The authors point to regional differences in smoking prevalence, dietary patterns, physical activity levels, and socio-economic determinants such as education and income inequality, all of which compound to affect mortality outcomes differently across regions. These social determinants of health influence both the onset and progression of diseases, perpetuating spatial disparities despite national-level efforts.
This research gains additional contemporary relevance as it situates Italy’s mortality dynamics in the context of recent events, including the COVID-19 pandemic. The authors cautiously discuss how the pandemic’s differential regional impact may further complicate mortality trajectories, potentially exacerbating existing inequalities. They underscore the necessity for ongoing monitoring and region-specific interventions tailored to the evolving demographic and epidemiological landscape.
Beyond its immediate geographic focus, the study provides a rich framework for understanding mortality convergence (and divergence) phenomena in advanced economies more broadly. The methodological rigor and integration of demographic, epidemiological, and socio-economic data illustrate how nuanced analyses are essential to capture complex population health transitions. This work challenges simplistic narratives of steady mortality improvement and regional equality, urging more granular policy responses.
The findings have profound implications for regional development strategies and healthcare resource allocation within Italy. Recognizing that uniform policy prescriptions may be insufficient, the authors advocate for more calibrated and regionally informed interventions designed to address specific mortality drivers. Such policies could include enhanced chronic disease management programs, targeted prevention campaigns, and investments in healthcare infrastructure in lagging regions.
Furthermore, the study sparks a compelling dialogue about the sustainability of gains in population health amidst emerging social and economic challenges. Aging populations, shifting disease burdens, migration patterns, and climate change-related health risks all interact with regional mortality dynamics in complex ways. Understanding these interactions will be vital for shaping resilient public health frameworks.
In conclusion, the research spearheaded by Carboni and colleagues marks a pivotal moment in understanding Italy’s nuanced mortality landscape. By demonstrating the apparent end of the post-war era’s steady regional convergence in mortality, the study prompts a reassessment of health equity goals and the epidemiological future of the nation. It calls attention to the imperative of tailored, evidence-based policies that can address persistent inequalities and foster inclusive health improvements.
As Italy confronts these demographic challenges, the global scientific and public health communities will look to this research for insights into the mechanisms driving regional disparities in mortality, as well as for strategies to promote healthier populations more equitably. The evolving story of Italy’s mortality trends offers a template for other countries grappling with similar issues, emphasizing the critical intersection of demography, health policy, and socio-economic context in shaping population outcomes.
Subject of Research:
Mortality evolution and regional convergence trends in Italy.
Article Title:
Mortality evolution in Italy: the end of regional convergence?
Article References:
Carboni, G., Salinari, G., De Santis, G. et al. Mortality evolution in Italy: the end of regional convergence?. Genus 80, 28 (2024). https://doi.org/10.1186/s41118-024-00237-w
Image Credits:
AI Generated