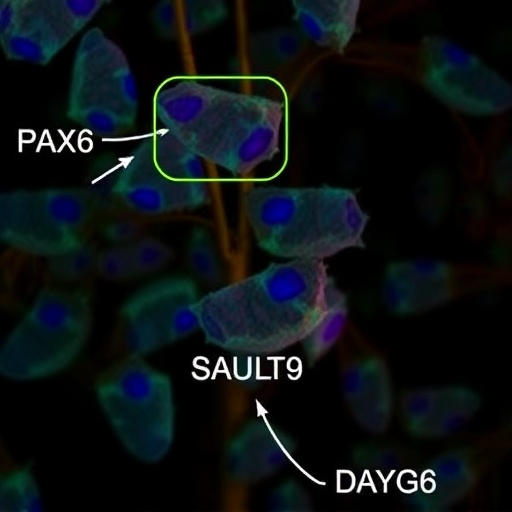
In a groundbreaking study published in Translational Psychiatry in 2025, scientists have unveiled a novel biomarker that could revolutionize the diagnosis and treatment of major depressive disorder (MDD). This discovery pivots on an unexpected player in the complex neuroimmune landscape: PAX6, a transcription factor predominantly known for its roles in neural development, but now identified as critically expressed in leukocytes of individuals suffering from MDD. The integration of neuroimmunology with psychiatric research opens unprecedented avenues for understanding the pathophysiology of depression and tailoring precision medicine approaches.
Major depressive disorder, affecting hundreds of millions worldwide, has traditionally been diagnosed through clinical interviews and symptom checklists, leading to often delayed or inadequate treatment responses. This study disrupts that paradigm by associating peripheral immune cells’ properties—specifically leukocytes expressing PAX6—with the central nervous system’s pathological state. This finding suggests that peripheral blood markers can reflect or even predict central neuropsychiatric conditions, a concept that could immensely simplify and objectify diagnosis.
PAX6, a paired box transcription factor extensively studied for its vital role in eye and brain development, had not previously been implicated in adult immune cells regarding psychiatric disorders. Dias et al. utilized cutting-edge integrative neuroimmunological methods to map gene expression patterns across both the central nervous system and peripheral blood samples, identifying a robust correlation between leukocyte PAX6 expression levels and depression phenotypes. This approach highlights the increasingly appreciated crosstalk between the immune system and brain function.
The researchers employed high-throughput RNA sequencing and single-cell transcriptomics to dissect leukocyte populations from cohorts of depressed patients and healthy controls. They discovered that subsets of immune cells, specifically certain leukocytes, exhibited significantly elevated PAX6 mRNA and protein expression in depressed individuals. This aberrant expression pattern correlated strongly with the severity of depressive symptoms, suggesting a potential mechanistic link rather than a mere epiphenomenon.
Further mechanistic investigations identified that leukocyte PAX6 plays a regulatory role in inflammatory signaling pathways known to affect neural plasticity and mood regulation. By modulating cytokine production and neuroinflammatory responses, PAX6-positive leukocytes might contribute directly to the neuropathological changes observed in MDD. These findings bridge a crucial gap between systemic immune dysregulation and neuropsychiatric symptomatology, affirming the long-suspected immune involvement in depression.
Importantly, the study’s longitudinal design showed that PAX6 expression levels in patient leukocytes could predict relapse and treatment response, making this marker not only diagnostic but also prognostic. Patients with persistently high leukocyte PAX6 levels were less likely to respond favorably to standard antidepressants, indicating a potential for tailoring personalized treatments based on immune profiling. This could usher in an era of precision psychiatry where molecular biomarkers guide therapeutic decisions.
The integration of neuroimmunology into psychiatric research reflects a broader trend in the field, where the brain is no longer considered in isolation. Instead, it is increasingly viewed as part of a dynamic system involving peripheral immune cells, the microbiome, and the endocrine system. This study exemplifies how such integrative approaches can uncover unexpected pathological mechanisms, challenging conventional wisdom and opening new therapeutic vistas.
Given the complexity of MDD, the identification of leukocyte PAX6 as a critical predictor underscores the importance of cross-disciplinary collaboration. The research team paired expertise spanning neurobiology, immunology, psychiatry, and bioinformatics to unravel this multifaceted problem. Their interdisciplinary methodology sets a new standard for future studies aiming to decode psychiatric disorders’ biological underpinnings.
The implications extend beyond diagnostics. By targeting leukocyte PAX6 or its downstream effectors, novel immunomodulatory treatments could be devised. Such therapies might circumvent the limitations of current antidepressants, which predominantly target neurotransmitter systems and often have delayed efficacy and side effects. Modulating immune pathways implicated in mood regulation could offer faster, more effective symptom relief.
Moreover, this research provides compelling evidence supporting the growing hypothesis that inflammation and immune dysfunction are not only consequences but also potential drivers of depressive pathology. Understanding the role of leukocyte transcription factors like PAX6 may help clarify the bidirectional relationship between mental health and systemic immunity, ultimately reducing stigma and fostering holistic treatment strategies.
The research team also explored how environmental factors known to influence both immunity and depression, such as stress and infection history, modulate PAX6 levels in leukocytes. These findings suggest that PAX6 expression could be a convergence point where genetic predispositions and external stressors intersect to influence disease trajectory—an insight that could guide preventive interventions.
The study’s methodological rigor, including replication in independent cohorts and multimodal validation, ensures robustness and generalizability of the findings. Furthermore, leveraging advanced bioinformatics to integrate transcriptomic data with clinical parameters exemplifies the power of big data in unraveling psychiatric disorders. Together, these strengths propel the findings towards clinical translation.
As the scientific community moves forward, incorporating peripheral immune markers like leukocyte PAX6 into routine psychiatric evaluation may become feasible, particularly with advances in minimally invasive blood sampling and molecular diagnostics. This is a promising step toward objective, biology-based psychiatry, moving away from subjective symptom-based diagnostics.
In summary, this innovative investigation into neuroimmune mechanisms uncovers leukocyte-expressing PAX6 as a groundbreaking biomarker and potential therapeutic target for major depressive disorder. Its findings underscore the intricate interaction between immune function and brain health, heralding a paradigm shift in how depression is understood and treated. As research follows suit, integrating molecular immunology into psychiatry could vastly improve patient outcomes and transform mental health care.
Subject of Research: Major depressive disorder and neuroimmunology, focusing on peripheral immune biomarkers.
Article Title: Integrative Neuroimmunology Reveals Leukocyte-Expressing PAX6 as a Critical Predictor of Major Depressive Disorder
Article References:
Dias, H.D., Adri, A.S., Nóbile, A.L. et al. Integrative neuroimmunology reveals leukocyte-expressing PAX6 as a critical predictor of major depressive disorder. Transl Psychiatry (2025). https://doi.org/10.1038/s41398-025-03776-8
Image Credits: AI Generated