In the United States, the landscape of sexual education remains a patchwork quilt of disparate legal mandates and educational policies, often lacking uniformity, scientific accuracy, and comprehensive scope. Recent research spearheaded by experts at Boston University School of Public Health reveals critical disparities in how sexual education is legislated and delivered across states, spotlighting profound implications for adolescent health and well-being nationwide. This intricate mosaic of state-driven mandates demonstrates that despite nearly universal requirements for some form of sexual education, the content’s accuracy, inclusivity, and scientific rigor vary dramatically, with many jurisdictions failing to meet the standards advocated by leading medical and public health authorities.
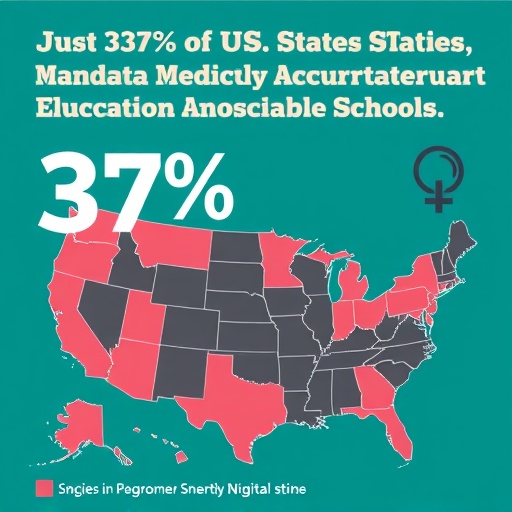
The absence of a federal mandate for sexual education in public schools engenders significant heterogeneity in curricular content from state to state. This decentralized governance means that each state’s legislature or education board interprets and implements sexual education policy in ways that can range from medically rigorous to ideologically driven, often influenced by political, cultural, and social factors. The study found that while 42 states compel public school students to receive some sexual education by the time they graduate high school, only 19 states require this instruction to be medically accurate. An even smaller number ensure that this accuracy spans the entirety of the curriculum, highlighting a pervasive gap in the reliability and quality of sexual health information provided in schools.
Among the mandated topics, abstinence receives disproportionate emphasis. Thirty-four states compel instruction on abstinence, despite compelling evidence from decades of public health research showing that abstinence-only education lacks efficacy in reducing rates of sexually transmitted infections (STIs), unintended pregnancies, or promoting healthy sexual behaviors. This preference is often intertwined with federal funding streams and local sociopolitical agendas that elevate abstinence-centric messaging over comprehensive sexual education models. The consequences of this are dire, as adolescents remain vulnerable to misinformation, stigma, and a lack of preparedness to make informed decisions about consent, contraception, and sexual health.
Parental rights heavily influence the delivery of sexual education, with 34 states allowing parents to opt their children out of these programs and five states requiring explicit opt-in consent. These opt-out and opt-in policies, while framed as protective measures for parental authority, often act as barriers to equitable access to medically accurate and inclusive sexual health education. They complicate efforts to reach at-risk adolescents who may require critical information for navigating relationships safely and understanding their bodies and rights. The study calls for further analysis to understand how these policies modulate the practical impact of sexual education mandates and potentially exacerbate health disparities.
Geographically, the Northeast region emerges as the most consistent in mandating sexual education with at least basic topic coverage, followed by the South, Midwest, and West, though the comprehensiveness and accuracy of these curricula remain uneven across all regions. Such regional disparities reflect underlying cultural, political, and demographic factors that shape educational priorities and public health strategies in each state. This regional variation underscores the need for nuanced policy interventions that consider localized contexts while advocating for nationwide standards anchored in scientific evidence.
The content requirements of sexual education vary widely and often omit critical topics essential for fostering a holistic understanding of sexual health. While topics such as HIV/AIDS and sexually transmitted infections feature prominently, other crucial areas such as contraception, sexual orientation, condom use, and the concept of consent receive markedly less legislative endorsement. For instance, only 20 states mandate instruction on contraception, and even fewer require education about sexual orientation (12 states), condom use (11 states), or consent to sexual activity (9 states). This selective coverage neglects vital components of sexual health literacy necessary for reducing risk and promoting healthy relationships among youth.
More alarming is the presence of stigmatizing and scientifically unsupported messaging within some state curricula. Two of the 12 states that require instruction on sexual orientation—Oklahoma and Texas—also necessitate the dissemination of negative messaging that inaccurately associates same-sex activity with heightened AIDS exposure. Such content not only contravenes established scientific consensus but also perpetuates stigma and discrimination against LGBTQ+ youth, compounding their risk for adverse psychosocial and health outcomes.
The methodology underpinning this comprehensive content analysis involved an exhaustive examination of state statutes, administrative codes, and judicial decisions governing sexual education across all 50 states and Washington, D.C. This legal-analytical approach allowed researchers to map the regulatory terrain, identify content mandates, and assess the presence and scope of parental consent policies. Findings demonstrate that infrastructural legal frameworks lay the groundwork for educational disparities that limit adolescents’ access to comprehensive, scientifically grounded sexual education.
Experts emphasize that the sociopolitical environment within each state exerts enormous influence over sexual education content and policy trajectories. Vocal advocacy groups, political ideologies, and cultural values collectively shape legislative priorities, often resulting in the perpetuation of abstinence-focused and exclusionary curricula despite growing evidence supporting the efficacy of comprehensive sexual health education. This intersection of politics and pedagogy emphasizes the complexity of reform efforts intended to enhance sexual education nationwide.
Adolescents face disproportionate risks related to sexual health, including infection with HIV and other STIs, unintended pregnancies, and exposure to unhealthy interpersonal dynamics such as intimate partner violence and sexual assault. The failure to equip young people with medically accurate, inclusive, and comprehensive information exacerbates these risks and undermines public health objectives. Consequently, the study’s findings carry significant implications for policymakers, educators, and public health practitioners mobilizing to improve adolescent health through evidence-based educational initiatives.
The research team, which includes scholars from Boston University School of Public Health, Cornell Law School, and Florida International University, advocates for expanded policy reforms driven by up-to-date scientific understanding and public health best practices. Such reforms would ideally reconcile state-level regulatory fragmentation by standardizing content requirements that promote accuracy, inclusivity, and comprehensiveness, ensuring all students receive education that reflects current scientific consensus and addresses diverse student needs.
This study, published in the American Journal of Public Health, represents a critical step toward illuminating the legislative underpinnings of sexual education disparities and identifies clear avenues for policy advancement. Researchers hope these insights will catalyze efforts toward harmonizing educational standards, dismantling entrenched ideological barriers, and fostering an environment where evidence-based sexual health education becomes the norm rather than the exception.
Ultimately, advancing sexual education policy in the United States hinges not only on legislative will but also on societal acknowledgment of adolescent health needs and the moral imperative to provide youth with the tools necessary to navigate their sexual lives safely and responsibly. By confronting the existing regulatory shortcomings illuminated by this research, stakeholders can better align sexual education with the overarching goals of public health, equity, and youth empowerment.
Subject of Research: Not applicable
Article Title: The State of Sexual Education: State Laws and Regulations Mandating Sexual Education in the United States
News Publication Date: August 22, 2025
Web References:
https://ajph.aphapublications.org/doi/10.2105/AJPH.2025.308199
https://www.who.int/news-room/questions-and-answers/item/comprehensive-sexuality-education
https://www.cdc.gov/youth-behavior/risk-behaviors/sexual-risk-behaviors.html
https://oklahoma.gov/health/services/personal-health/sexual-health-and-harm-reduction-service/educators/hiv-education-training-het.html
References:
Nelson, K., Underhill, K., et al. (2025). The State of Sexual Education: State Laws and Regulations Mandating Sexual Education in the United States. American Journal of Public Health, DOI:10.2105/AJPH.2025.308199.
Keywords:
Sex education, Human sexual behavior, Sexuality, Infectious diseases, Sexually transmitted diseases, HIV research, Adolescents, Public health, High school education