In a groundbreaking case report recently published in BMC Psychiatry, researchers document an unprecedented co-occurrence of isovaleric acidemia (IVA) with schizophrenia, shedding light on complex interactions between rare metabolic disorders and severe psychiatric conditions. This remarkable report explores the clinical presentation, therapeutic interventions, and potential pathophysiological pathways linking these two seemingly distinct entities.
Schizophrenia, a debilitating and chronic psychiatric disorder affecting approximately 1% of the global population, is typified by hallucinations, delusions, and disorganized thought and behavior. These symptoms reflect profound neurochemical and neurodevelopmental dysregulation, yet its exact etiology remains elusive, with genetic, environmental, and neurobiological components historically implicated. This new case introduces an intriguing metabolic dimension to the schizophrenia landscape, through the rare inherited metabolic disease isovaleric acidemia.
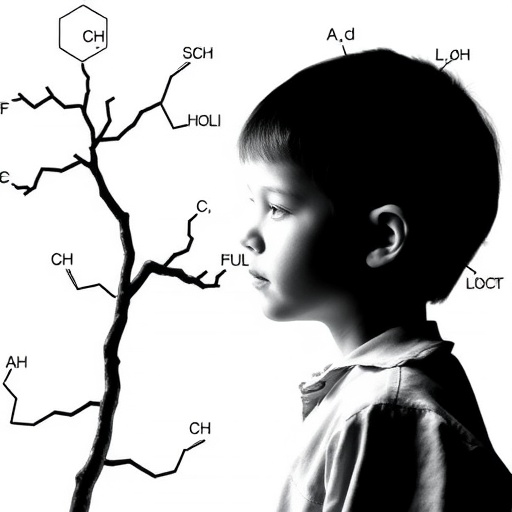
Isovaleric acidemia arises from a deficiency in isovaleryl-CoA dehydrogenase, an enzyme critical in the catabolism of the amino acid leucine. This enzymatic block results in the toxic accumulation of isovaleric acid and related metabolites, leading to a spectrum of clinical manifestations ranging from acute metabolic crises to chronic neurodevelopmental impairments. Because IVA is exceptionally rare, with incidence estimated between 1 in 250,000 to 1 in 500,000 live births, its interface with psychiatric illness has remained largely unexplored until now.
The reported case involves a 25-year-old male patient diagnosed with both IVA and schizophrenia, who presented at a psychiatric facility with escalating auditory hallucinations and paranoid delusions. His psychiatric deterioration prompted a multidisciplinary approach, combining antipsychotic treatment with targeted metabolic therapies. Notably, clozapine at 150 mg/day and blonanserin at 24 mg/day were administered to mitigate psychotic symptoms, while metabolic management included L-carnitine at 3 g/day and reduced glutathione at 1.2 g/day to address the underlying metabolic dysfunction.
Therapeutic outcomes revealed partial remission: auditory hallucinations completely abated under this dual regimen, whereas delusional thought patterns, although decreased in severity, persisted. This partial response underscores the intricate interplay between metabolic dysregulation and psychosis, suggesting that conventional psychiatric treatments may require adjunctive metabolic support in such complex cases.
The biochemical basis underlying IVA’s potential contribution to schizophrenia pathology is hypothesized to involve neurotoxic effects of accumulated isovaleric acid and its derivatives, which may disrupt neurotransmitter synthesis, oxidative stress balance, and neuronal viability. Such disruptions could feasibly precipitate or exacerbate psychotic symptomatology by altering dopaminergic and glutamatergic pathways, which are central to schizophrenia’s neurobiology.
Moreover, the case report propounds that chronic metabolic stress and neuroinflammation resulting from IVA might serve as environmental insults that interact synergistically with genetic predisposition to lower the threshold for schizophrenia onset. This multifactorial model aligns with emerging paradigms emphasizing metabolic and immune contributions to psychiatric disorders, thus broadening the conceptual framework for schizophrenia’s etiology.
The rarity of simultaneous IVA and schizophrenia diagnosis has previously hindered systematic investigation; therefore, this clinically detailed case provides a valuable foundation for future research aimed at corroborating causative mechanisms and optimizing therapeutic strategies. Understanding the metabolic-psychiatric nexus could herald personalized medicine approaches that target biochemical abnormalities alongside neurochemical imbalances.
Importantly, this report highlights the need for heightened clinical awareness and comprehensive metabolic evaluation in patients presenting with atypical or treatment-resistant psychosis. Early identification of hidden metabolic disorders like IVA may facilitate timely intervention, potentially improving psychiatric outcomes and reducing morbidity associated with delayed diagnosis.
Furthermore, the pharmacological combination utilized in this case illustrates the feasibility and potential efficacy of integrating metabolic and psychiatric treatments. L-carnitine, a cofactor in fatty acid oxidation, and reduced glutathione, a potent antioxidant, may counteract mitochondrial dysfunction and oxidative stress—pathways increasingly recognized in both metabolic and neuropsychiatric disorders, further supporting their adjunctive role.
This case also poses compelling questions regarding the long-term prognosis of patients with dual IVA and schizophrenia diagnoses. Longitudinal studies are warranted to elucidate the trajectory of psychiatric symptoms in the context of metabolic control and to establish evidence-based guidelines for integrated care.
In conclusion, the reported coexistence of isovaleric acidemia with schizophrenia invites a paradigm shift by bridging metabolomics and psychiatry. This intersection points to a novel dimension of schizophrenia pathophysiology, emphasizing that rare metabolic disorders might not only manifest neurological symptoms but also contribute directly to complex psychiatric phenotypes. Such insights pave the way for transformative research and clinical practices, ultimately enhancing patient outcomes in this challenging clinical landscape.
Subject of Research:
A rare case detailing the comorbidity of isovaleric acidemia and schizophrenia, investigating clinical presentation, treatment, and underlying metabolic-psychiatric interactions.
Article Title:
A rare case of isovaleric acidemia and schizophrenia: a case report
Article References:
Zhou, J., Chen, H., Chen, X. et al. A rare case of isovaleric acidemia and schizophrenia: a case report. BMC Psychiatry 25, 897 (2025). https://doi.org/10.1186/s12888-025-07239-8
Image Credits: AI Generated
DOI:
https://doi.org/10.1186/s12888-025-07239-8