In recent years, the intricate relationship between inflammation and depression has increasingly drawn the attention of neuroscientists and psychiatrists alike. A groundbreaking study published in Translational Psychiatry has now shed new light on how systemic inflammation, brain perfusion abnormalities, and clinical characteristics collectively influence the persistence and treatment outcomes of depression. This longitudinal investigation offers compelling evidence that integrating biological and neuroimaging biomarkers could revolutionize the personalized management of inflammatory depression, signaling a crucial advancement in psychiatric research.
Depression, a multifaceted mood disorder affecting millions worldwide, demonstrates significant heterogeneity in symptoms and treatment responses. While traditional approaches have primarily focused on neurotransmitter imbalances and psychological factors, this emerging research underscores the critical role inflammation might play as a pivotal pathophysiological mechanism. The study meticulously explores how elevated levels of systemic inflammation, marked by C-reactive protein (CRP), correlate with brain perfusion irregularities and how these factors jointly forecast depressive trajectories over a six-month period.
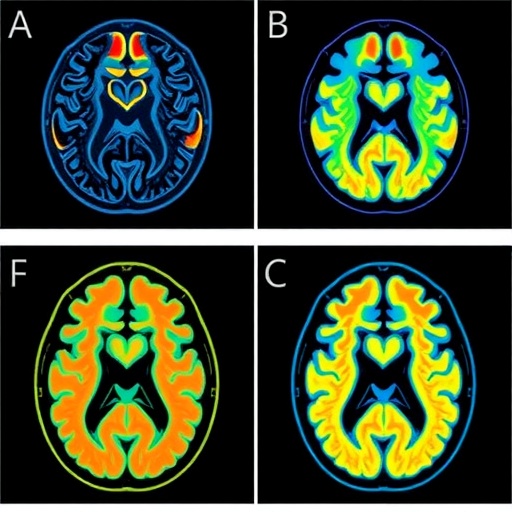
Leveraging advanced MRI perfusion imaging, the researchers pinpointed alterations in cerebral blood flow specifically within neural circuits governing emotion regulation and decision-making—two domains profoundly disrupted in depression. Areas such as the prefrontal cortex and anterior cingulate cortex, known for their involvement in mood modulation and cognitive control, exhibited distinctive perfusion patterns correlating with inflammation markers. These neurovascular imbalances potentially elucidate underlying mechanisms contributing to persistent depressive symptoms, including anhedonia and impaired reward processing.
The study was characterized by an integrative approach combining biochemical assays with sophisticated neuroimaging techniques to comprehensively assess participants’ inflammatory profiles and cerebral perfusion status at baseline. Over six months, participants’ depressive symptoms were continuously monitored, allowing the research team to evaluate how initial biomarker statuses predicted clinical outcomes, including treatment resistance and depression persistence. This multidimensional design represents a significant stride toward biomarker-informed psychiatric diagnostics.
One salient finding is the robust association between higher baseline CRP levels and poorer depression outcomes. CRP, a hallmark of systemic inflammation, was not merely a peripheral indicator but showcased a strong predictive capacity when analyzed alongside brain perfusion data. This intersection signifies the relevance of inflammatory processes in brain function deregulation, offering a plausible link that underpins why some patients remain resistant to conventional antidepressant therapies.
Crucially, the study also identified that certain clinical variables, notably younger age and longer duration of the depressive episode at baseline, synergistically augmented prediction models for treatment resistance. These clinical factors, amalgamated with biomarker information, underscore the necessity of individualized assessments surpassing symptom rating scales alone. This approach aligns with precision psychiatry paradigms aimed at customizing treatments based on a patient’s unique biological and clinical signatures.
The researchers emphasized the ramifications of these insights for the conceptualization of ‘inflammatory depression’ as a distinct subtype, characterized by its neuroimmune pathology and distinct neuroimaging signature. This subtype likely demands targeted therapeutic interventions addressing inflammatory cascades alongside traditional psychopharmacology, raising prospects for novel anti-inflammatory treatments or neurovascular restorative strategies in psychiatry.
Observing altered perfusion in reward-related brain regions offers a mechanistic explanation for anhedonia, a cardinal symptom often refractory to standard antidepressants. The diminished cerebral blood flow may reflect or precipitate synaptic and neuronal dysfunction, highlighting how systemic inflammation may translate into tangible brain circuit disruptions that sustain depressive syndromes. This neurological insight bridges peripheral immune status and central nervous system pathology.
The study also raises intriguing questions about the directionality and causality within the inflammation-depression axis. While elevated CRP and perfusion anomalies predict worse outcomes, discerning whether inflammation initiates these brain changes or exacerbates pre-existing vulnerabilities warrants further exploration. Nevertheless, these findings support the hypothesis that neuroinflammation forms a crucial intervening variable influencing treatment responsiveness and clinical trajectories.
By incorporating both biological markers and brain imaging data, this integrative framework introduces an advanced biomarker toolkit that could refine clinical decision-making. Clinicians armed with such predictive tools might better stratify patients for specific treatments, foresee chronicity risks, and ultimately improve prognosis. This marks a departure from one-size-fits-all modalities, steering the field toward stratified medicine tailored to underlying pathophysiological mechanisms.
Looking ahead, the authors advocate for validation studies in larger, more diverse cohorts to generalize these findings and embed them into clinical protocols. Expanding biomarker panels and refining neuroimaging techniques could further enhance predictive accuracy. Furthermore, interventional trials targeting inflammation—whether through pharmacological agents or lifestyle modifications—remain vital next steps to confirm causal inferences and therapeutic potential.
The implications of this research extend beyond clinical practice into the broader understanding of depression’s neurobiology. By elucidating how systemic inflammation interfaces with brain perfusion anomalies, the study propels the notion that depression encompasses somatic and neural dimensions interwoven through the immune system. Such holistic perspectives pave the way for multi-modal interventions embracing neuroimmune targets.
Moreover, this investigation contributes to the evolving narrative that brain imaging biomarkers possess vital roles beyond diagnostics, serving as dynamic indicators of disease activity and treatment efficacy. The ability to non-invasively monitor cerebral perfusion changes linked to clinical states and inflammatory status opens avenues for real-time management adjustments and personalized monitoring in psychiatric care.
Intriguingly, the study’s multidimensional approach could inspire analogous frameworks for other neuropsychiatric disorders with inflammatory components, such as bipolar disorder, schizophrenia, and neurodegenerative diseases. The cross-disciplinary methodologies combining neuroimaging, immunology, and clinical phenotyping set a new standard for integrative brain research.
In conclusion, this longitudinal study represents a landmark effort in characterizing inflammatory depression through convergent lines of evidence encompassing biomarkers and neuroimaging. By demonstrating how systemic inflammation and cerebral perfusion abnormalities intertwine with clinical characteristics to predict depressive outcomes, it elevates the promise of precision psychiatry. As science moves toward unraveling depression’s complex neuroimmune landscape, such integrative research heralds innovative, targeted therapeutic avenues poised to transform mental health care.
Subject of Research: The study investigates the interplay between systemic inflammation, brain perfusion abnormalities, and clinical factors in predicting the persistence and treatment resistance of depression.
Article Title: Inflammatory and MRI perfusion biomarkers in predicting persistence of depression: a 6-month Longitudinal Study
Article References:
Batail, JM., Corouge, I., Blanchard, T. et al. Inflammatory and MRI perfusion biomarkers in predicting persistence of depression: a 6-month Longitudinal Study. Transl Psychiatry 15, 370 (2025). https://doi.org/10.1038/s41398-025-03587-x
Image Credits: AI Generated