In a groundbreaking study poised to reshape the landscape of colon cancer diagnostics and therapeutics, researchers have unveiled compelling evidence positioning IL22RA1 as a potent biomarker and therapeutic target in the progression of human colon cancer. Given that colon cancer remains a global health challenge, ranking persistently among the top three cancers in both incidence and mortality, the need for novel indicators that could predict disease course and patient outcomes is more urgent than ever.
Colon cancer’s clinical management has traditionally relied on surgical intervention accompanied by adjuvant chemotherapy and radiotherapy. Although immunotherapy has revolutionized treatment paradigms for various malignancies, only a minority of colon cancer patients experience significant benefits. This limitation has fueled intense investigation into the molecular underpinnings and immune microenvironment of colon cancer, aiming to uncover new therapeutic targets capable of altering prognosis and treatment responsiveness.
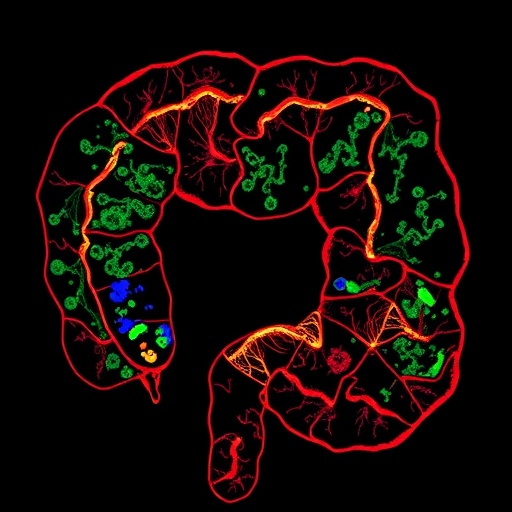
The investigators employed sophisticated multi-color immunohistochemistry (mIHC) techniques combined with multispectral tissue imaging to dissect the expression landscapes of IL22RA1 and its associated molecules IL22, CD155, and IL22BP within a well-characterized tissue microarray of 90 colon cancer specimens. Notably, IL22RA1 emerged predominantly within tumor epithelial cells, underscoring its potential role at the frontline interface between malignant cells and the immune milieu.
Quantitative assessments revealed significantly elevated levels of IL22RA1, CD155, and IL22BP in tumor tissues compared to adjacent normal mucosa, with statistical analyses confirming the robustness of these differences. This differential expression illuminates a possible contributory role of these molecules in creating an immunologically permissive tumor microenvironment that may facilitate cancer progression and immune evasion mechanisms.
Correlative clinical data further strengthened the prognostic relevance of IL22RA1. Patients exhibiting low IL22RA1 expression demonstrated markedly improved overall survival compared to their high-expression counterparts, suggesting that IL22RA1 could serve as a reliable biomarker for stratifying patients based on risk. The prognostic impact intensifies when considering combinatorial expression profiles: individuals with concurrent high expression of IL22RA1 and IL22, or IL22RA1 and CD155, experienced significantly poorer survival outcomes, implicating a synergistic effect between these molecules in promoting tumor aggressiveness.
An intriguing inverse correlation surfaced between IL22RA1 and IL22BP expressions, where patients with low IL22RA1 and high IL22BP expression patterns enjoyed more favorable survival. This relationship hints at a complex regulatory axis within the tumor microenvironment, with IL22BP potentially acting as a natural antagonist to IL22 signaling and counterbalancing the deleterious effects driven by IL22RA1 overexpression.
Further statistical rigor was applied through Cox multivariate regression, which identified high IL22RA1 expression as an independent prognostic risk factor, conferring a hazard ratio exceeding 2.7. This finding confirms that beyond established clinical parameters, IL22RA1 levels in tumor cells carry significant predictive power for patient outcomes, underscoring its utility for personalized medicine approaches.
The study also delved into the immune cell infiltrate dynamics against the backdrop of IL22RA1 expression. Tumors with elevated IL22RA1 expression featured markedly reduced infiltration of crucial T cell subsets, particularly central memory CD8+ T cells and memory CD4+ T cells, pivotal components of sustained immune surveillance and antitumor response. This depletion suggests IL22RA1 may orchestrate immunosuppressive conditions, enabling tumor cells to escape immune detection and destruction.
At the molecular interface, IL22RA1’s interaction with IL22 appears to fuel tumorigenesis, likely by activating downstream signaling pathways that promote proliferation and survival of malignant cells. The receptor’s association with CD155 — a molecule implicated in immune checkpoint modulation — further amplifies its role in sculpting an immune evasive niche favoring tumor persistence and progression.
These discoveries highlight the dual facets of IL22RA1 as both a marker of adverse prognosis and a potential linchpin in colon cancer’s immune evasion strategies. Therapeutically targeting IL22RA1 or disrupting its functional crosstalk with IL22 and CD155 could open new frontiers in colon cancer treatment, particularly for patients resistant to conventional immunotherapies.
Given these insights, IL22RA1 stands out not only as a prognostic biomarker but also as a promising candidate for the development of novel immunotherapeutic agents. Such approaches may involve antibody-based blockade, receptor antagonists, or small molecules designed to dismantle the deleterious signaling networks driven by IL22RA1.
Moreover, the robust correlation between IL22RA1+CK+ and CD155+CK+ tumor cell populations suggests a co-expression signature that could refine risk stratification models and guide therapeutic decisions. This phenotypic interplay within tumor epithelial compartments merits further exploration to uncover mechanistic details and identify synergistic intervention points.
The implications of these findings echo beyond colon cancer, inviting speculation about IL22RA1’s involvement in other malignancies characterized by immune dysregulation and chronic inflammation. Future research expanding upon these results may unravel broader paradigms of tumor-immune crosstalk mediated by IL22RA1, potentially impacting a wide range of cancer types.
In conclusion, this meticulous study illuminates the pivotal role of IL22RA1 in colon cancer progression and patient survival, providing a compelling rationale for integrating IL22RA1 assessment into clinical workflows. As research advances, harnessing the therapeutic potential of targeting IL22RA1 may herald a new chapter in combating this formidable disease, turning what was once an intractable prognosis into a manageable clinical reality.
Subject of Research: Expression and clinical significance of IL22RA1 and associated molecules in human colon cancer progression.
Article Title: Evaluating IL22RA1 expression as a predictive indicator in human colon cancer progression
Article References:
Yin, X., Geng, R., Chen, J. et al. Evaluating IL22RA1 expression as a predictive indicator in human colon cancer progression. BMC Cancer 25, 1278 (2025). https://doi.org/10.1186/s12885-025-14715-7
Image Credits: Scienmag.com