In a groundbreaking study poised to redefine our understanding of depression treatment, researchers have unveiled a compelling relationship between the structural integrity of the hippocampus and the therapeutic efficacy of escitalopram, a widely prescribed selective serotonin reuptake inhibitor (SSRI). This revelation, published in Translational Psychiatry in early 2025, offers new hope for personalized interventions in major depressive disorder (MDD), a condition that afflicts millions globally and often resists conventional therapies.
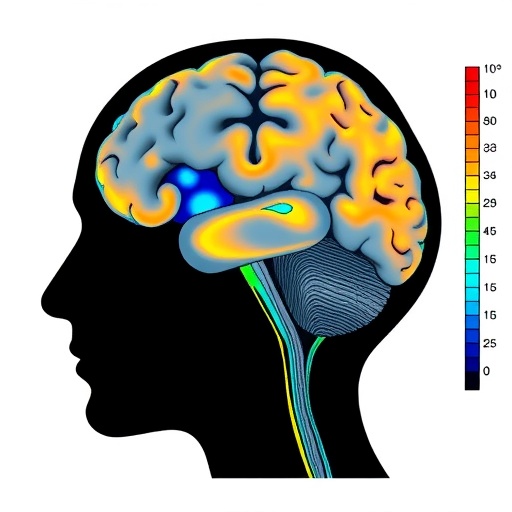
Depression’s neurobiological underpinnings have long been the subject of intense scientific scrutiny, with the hippocampus—a crucial brain region involved in memory, emotion regulation, and neuroplasticity—emerging as a key player. Previous studies have suggested that decreased hippocampal volume correlates with depression severity and recurrence, but the direct impact of antidepressant treatment on hippocampal morphology, and how this morphological change relates to therapeutic outcomes, remained elusive until now.
The research team, led by Kamishikiryo et al., leveraged high-resolution MRI imaging to longitudinally track hippocampal volume changes in patients diagnosed with MDD before and after a regimented course of escitalopram. Utilizing standardized volumetric analysis combined with clinical scales assessing depression severity, their methodical approach enabled a granular correlation between anatomical change and symptom improvement.
Crucially, their findings demonstrated that responders to escitalopram exhibited significant hippocampal volume increases post-treatment, suggesting a robust neuroplastic response. This volume augmentation was not merely a side effect but appeared tightly coupled to symptomatic relief, underlining the hippocampus’s role as a biomarker for antidepressant responsiveness. Conversely, non-responders showed negligible volumetric changes, highlighting potential neural deficits that escape escitalopram’s pharmacodynamic influence.
Escitalopram exerts its antidepressant effect primarily through potentiation of serotonergic signaling pathways, enhancing synaptic availability of serotonin which modulates mood and cognition. The neurotrophic consequences of these biochemical shifts likely promote neurogenesis and dendritic remodeling within the hippocampus, possibly underpinning the observed volumetric expansions. These mechanisms align with the neurogenic hypothesis of depression, positing that therapeutic efficacy depends, at least in part, on restoration of hippocampal neuron proliferation and connectivity.
Delving deeper into the temporal dynamics, the study meticulously documented that hippocampal volume increases became statistically significant only after several weeks of continuous escitalopram administration, mirroring the typical delayed onset of clinical antidepressant effects. This parallelism reinforces the notion that structural brain changes are not incidental but integral to the therapeutic timeline and efficacy.
Furthermore, the investigation accounted for confounding variables including age, illness duration, baseline depression severity, and comorbidities, ensuring the observed hippocampal volumetric changes were attributable to treatment response rather than external factors. This rigorous control enhances the study’s validity and provides a solid platform for translating these findings into clinical practice.
The implications of this research are profound: assessing hippocampal volume prior to treatment could feasibly serve as a predictive biomarker, enabling clinicians to tailor antidepressant choices and dosages more effectively. Early identification of likely non-responders could prompt alternative therapeutic strategies, such as adjunctive psychotherapy or novel pharmacological agents, optimizing patient outcomes and reducing the trial-and-error approach that currently characterizes depression management.
Moreover, the neuroplasticity observed in escitalopram responders invites future exploration into adjunctive therapies that may potentiate hippocampal recovery, including cognitive-behavioral therapy, exercise, and emerging neuromodulation techniques like transcranial magnetic stimulation (TMS). Integrating structural brain monitoring into clinical protocols could thus revolutionize how depression treatments are administered and evaluated.
It is also noteworthy that this research intersects with the burgeoning field of precision psychiatry, emphasizing biological heterogeneity within psychiatric disorders. Depression is increasingly understood not as a unitary entity but as a spectrum of subtypes with distinct pathophysiologies. Hippocampal volume assessment may carve out a neuroanatomical subtype responsive to SSRIs, guiding more nuanced therapeutic stratification.
Despite these promising advances, the authors caution that hippocampal volumetric measurement via MRI entails logistical and financial challenges limiting widespread clinical adoption at present. Future work is needed to validate these findings across larger, more diverse populations and to develop streamlined imaging protocols compatible with routine outpatient settings.
In summary, this seminal study by Kamishikiryo and colleagues elucidates an essential link between hippocampal structure and antidepressant response, enriching our neurobiological comprehension of depression and opening avenues for personalized medicine. Escitalopram’s ability to induce hippocampal volume increases in responders underscores the brain’s remarkable capacity for plasticity and recovery, offering renewed optimism for those battling this debilitating condition.
As psychiatric research progresses, integrating anatomical biomarkers with genetic, molecular, and behavioral data will likely sharpen diagnostic precision and treatment effectiveness. This multifaceted approach heralds a future where depression is tackled not only as a clinical syndrome but as a biologically defined disorder, uniquely tailored to each patient’s neuroprofile.
For clinicians, patients, and researchers alike, these findings underscore the imperative to rethink depression treatment paradigms through the lens of brain plasticity and structural neuroscience. The hippocampus, once known primarily for memory functions, now emerges as a linchpin in the fight against depression, symbolizing the convergence of mind and brain in mental health recovery.
As the field advances, the question remains: could routine hippocampal volume assessment become a gold standard in psychiatric care, transforming how millions receive relief from depression? While hurdles persist, the path illuminated by Kamishikiryo et al. signals a pivotal shift towards biologically informed, patient-centered treatment strategies.
In the wake of this transformative research, the scientific community eagerly anticipates further studies to delineate the precise molecular cascades linking escitalopram’s serotonin modulation to hippocampal neuroplasticity. Such insights will propel the development of next-generation antidepressants and adjunctive therapies aimed at amplifying brain resilience.
Ultimately, this landmark study not only reshapes our understanding of antidepressant action but also fuels hope for more effective, enduring solutions to one of the world’s most pervasive mental health challenges.
Subject of Research: The study investigates the relationship between hippocampal volume and the treatment response to escitalopram in patients with depression.
Article Title: Relationship between hippocampal volume and treatment response before and after escitalopram administration in patients with depression.
Article References:
kamishikiryo, T., itai, E., mitsuyama, Y. et al. Relationship between hippocampal volume and treatment response before and after escitalopram administration in patients with depression. Transl Psychiatry (2025). https://doi.org/10.1038/s41398-025-03796-4
Image Credits: AI Generated