A team of researchers at the San Raffaele-Telethon Institute for Gene Therapy (SR-Tiget) in Milan, Italy, has made significant strides in the field of gene therapy, particularly focused on hematopoietic stem cells. Their recent findings suggest that there exists a critical window shortly after birth where these blood stem cells, which circulate in the bloodstream, can be targeted for gene therapy with enhanced effectiveness. This groundbreaking study, published in the prestigious journal Nature, provides a potential alternative treatment approach for genetic blood disorders, potentially eliminating the need for conventional stem cell transplantation or chemotherapy, which can be invasive and fraught with complications.
Historically, gene therapy using lentiviral vectors has demonstrated notable successes when performed ex vivo, where a patient’s stem cells are extracted, modified in a laboratory setting, and then reinfused after undergoing chemotherapy. One prominent example of this application is the therapy for metachromatic leukodystrophy (MLD), developed at SR-Tiget and approved in Europe and the United States. However, while this methodology has proven effective, it is also resource-intensive and presents challenges regarding patient comfort and treatment accessibility.
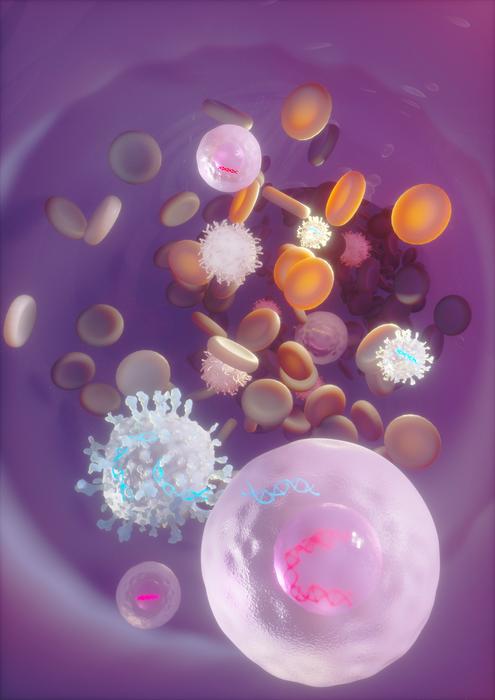
The innovative approach detailed in the recent study diverges from traditional practices by administering lentiviral vectors directly into the bloodstream in vivo. This method takes advantage of the unique physiological circumstances present in newborn mice. It was observed that during the first two weeks of life, the numbers of hematopoietic stem and progenitor cells (HSPCs) circulating in the bloodstream significantly surpass those found in older animals. This elevated presence of stem cells provides a critical window for gene transfer through systemic injection, facilitating long-term engraftment and the production of multilineage blood cells.
Dr. Michela Milani, the study’s lead author, articulated the significance of these findings by emphasizing the journey of blood stem cells post-birth. According to her, after birth, these stem cells must migrate from the liver—where they reside during the latter stages of pregnancy—to their permanent location in the bone marrow. This journey through the bloodstream creates an unparalleled opportunity for intravenous delivery of gene-modifying vectors, allowing for genetic alterations without the need for prior harvesting or lab processing of the cells.
To substantiate their research further, the team tested their novel in vivo gene transfer approach in mouse models simulating three distinct genetic disorders: adenine deaminase-deficient severe combined immunodeficiency (ADA-SCID), autosomal recessive osteopetrosis, and Fanconi anemia. In all three scenarios, the application of gene transfer was found to yield considerable therapeutic benefits. Notably, in the model pertaining to Fanconi anemia, corrected stem cells were able to progressively repopulate the blood system, thus averting the onset of bone marrow failure. This outcome closely mirrors what has been observed in human gene therapy studies wherein corrected cells demonstrate a survival and growth advantage over defective counterparts.
The researchers also aimed to enhance the effectiveness of gene transfer by utilizing clinically approved mobilizing agents such as G-CSF and Plerixafor. These substances were employed to dislodge stem cells from their tissue niches, ultimately resulting in an increased population of circulating stem cells and extending the potential treatment window to include older mice. Furthermore, the team optimized the lentiviral vectors to bolster their stability and improve cellular uptake—contributing to greater gene transfer efficiencies.
Significantly, the researchers detected HSPCs circulating in the blood of human newborns during the early months of life, which aligns with their earlier observations in mouse models. This finding reinforces the prospect that a similar opportunity for gene therapy may broadly exist in human populations. Dr. Alessio Cantore, another prominent figure in the study, remarked on the implications of their findings, suggesting that they provide proof of principle that in vivo lentiviral gene delivery is feasible during a crucial early-life window. If confirmed in human neonates, this method could have substantial implications for treating genetic diseases like severe immunodeficiencies and Fanconi anemia.
Moreover, the researchers noted an intriguing contrast in the behavior of stem cells between young and adult organisms. When stem cells are harvested from the blood of adult mice or humans, even with the aid of mobilizing drugs, they typically require additional activation signals to facilitate effective lentiviral gene transfer. Conversely, at the newborn stage, not only is there a greater abundance of circulating stem cells, but those cells also exhibit a higher degree of responsiveness to gene transfer efforts. This biological distinction underscores the necessity for further investigations into the mechanisms that govern this increased permissiveness in younger organisms, with aspirations to translate these findings to older age groups.
In conclusion, the research conducted by the SR-Tiget team illuminates a potentially transformative paradigm in the treatment of genetic blood disorders. By harnessing the properties of blood stem cells during a critical developmental window, they have opened a new avenue for therapeutic intervention that could refine and elevate the standard of care for patients burdened by genetic abnormalities. The implications of these findings not only underscore the importance of timing in medical treatments but also mark a pivotal advancement in the burgeoning field of gene therapy.
Subject of Research: Gene therapy targeting hematopoietic stem cells
Article Title: In Vivo Hemopoietic Stem Cell Gene Therapy Enabled by Post-Natal Trafficking
News Publication Date: 28-May-2025
Web References: Nature
References: 10.1038/s41586-025-09070-3
Image Credits: Ella Maru Studio
Keywords
Gene therapy, hematopoietic stem cells, lentiviral vectors, ex vivo, in vivo, genetic disorders, neonatal blood circulation, SR-Tiget, Milan, bone marrow failure, adenine deaminase-deficient severe combined immunodeficiency (ADA-SCID), gene transfer efficiency.