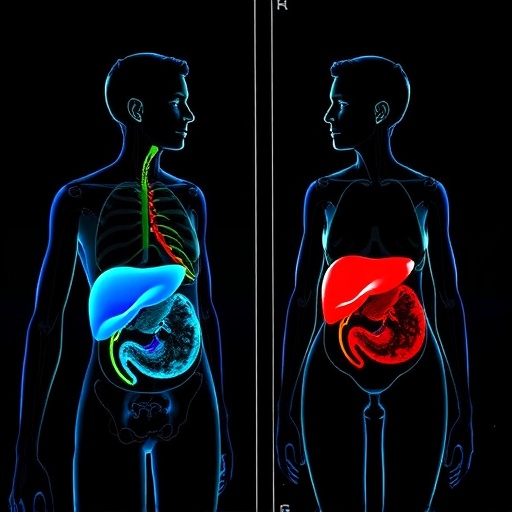
In a groundbreaking study, Aristu-Zabalza, Andrés-Rozas, Boyer-Díaz, and their collaborators illuminate crucial sex-specific differences in preclinical models related to advanced chronic liver disease and portal hypertension. This innovative research promises a significant advancement in the understanding of how gender influences pathophysiological mechanisms underlying liver disorders. Gender differences in disease manifestation have long been noted, but this work adds a new dimension by providing empirical data that could lead to better-targeted therapies.
The study builds upon a growing body of literature indicating that biological sex plays an essential role in the progression and treatment responses of chronic liver diseases. While many preclinical models typically utilize male subjects, the authors emphasize the necessity of incorporating female models to draw more accurate conclusions. A notable finding in their research was the marked differences in liver pathology and response to interventions between male and female subjects. This disparity calls into question the assumptions made in numerous previous studies that predominantly featured male participants.
A deeper dive into the study reveals the mechanisms through which sex hormones could be mediating the noted differences in liver disease progression. For instance, estrogen and testosterone have well-documented roles in modulating inflammatory responses and hepatic fibrosis. Aristu-Zabalza et al. meticulously examined the pathways through which these hormones influence liver function, yielding insights that could revolutionize therapeutic strategies. This understanding paves the way for novel therapeutic approaches that take into account the hormonal landscape of female patients, which has often been overlooked in clinical trials.
The researchers employed several state-of-the-art techniques to elucidate sex-specific responses to advanced chronic liver disease. By utilizing sophisticated animal models that mimic human pathophysiology, the authors examined key parameters such as liver inflammation, fibrosis progression, and portal pressure — each critical for understanding portal hypertension. Their work underscores the potential repercussions of failing to account for sex-specific differences, both in preclinical research and clinical practice.
This comprehensive analysis extends beyond just the biological functions of hormones; it dives into the genetic underpinnings that could contribute to variance in disease outcomes between sexes. The pivotal role of sex chromosomes and their interactions with environmental factors emerged as a central theme. The potential for genetic predispositions to influence the severity and type of liver disease presents an exciting avenue for further research.
The societal implications of this research cannot be overstated. Clinicians have a pressing responsibility to integrate findings from such studies into clinical practice. The discrepancies highlighted by this research could lead to misdiagnosis and suboptimal treatment for female patients suffering from hepatic diseases. The authors advocate for changes in clinical trial designs to ensure a more balanced representation of genders, thereby supporting more comprehensive and effective treatment protocols.
In their examination, Aristu-Zabalza et al. also discussed the role of lifestyle and environmental factors in exacerbating sex-specific differences. This aspect is crucial given the rising incidence of obesity-related liver diseases. A holistic approach that combines anatomical, physiological, and environmental factors related to gender could yield a more nuanced understanding of chronic liver diseases.
Critics of sex-specific research often raise concerns about potential gender biases that might overshadow men’s health issues. However, the authors vehemently counter this argument, elucidating the fact that understanding female specificities can only enhance overall healthcare. Improved strategies for treating liver diseases could ultimately lead to better health outcomes for all patients, irrespective of gender.
Moreover, the potential for personalized medicine emerging from these findings can transform how chronic liver diseases are managed. Tailoring treatment plans based on gender-related differences could not only improve efficacy but also reduce the risk of adverse side effects associated with one-size-fits-all approaches. The benefits are twofold: improved patient outcomes and optimized healthcare resources.
Education and outreach will also play a crucial role in embracing the findings of this study. Healthcare providers must be equipped with the knowledge to implement these insights effectively in their practices. Continuous professional development and training sessions tailored to understanding gender differences in chronic diseases should become a cornerstone of medical education moving forward.
The dialogue surrounding sex-specific research has the potential to influence public health policies as well. As monitoring and management of chronic liver diseases increasingly become focal points in healthcare systems globally, policy-makers need to consider the insights from studies like that of Aristu-Zabalza et al. Ensuring that research informs legislative decisions will be critical in addressing disparities that exist in liver disease care.
Lastly, the call for further investigations into sex-specific models of liver diseases cannot go unanswered. Future research must build upon the foundations laid by this study, expanding the understanding of how sex differences play into not just chronic liver diseases but a broader array of health conditions. As science continues to evolve, more nuanced research methodologies will be essential for exploring the complex interrelations between gender, genetics, environment, and health outcomes.
In conclusion, the work by Aristu-Zabalza and colleagues marks a pivotal moment in the exploration of sex-specific differences in liver diseases. As the medical community increasingly recognizes the importance of gender in health, this study serves as a clarion call for a transformation in research and clinical practice. The implications of these findings are vast, opening doors to enhanced therapies and improved healthcare delivery for all patients.
Subject of Research: Sex-specific differences in preclinical models of advanced chronic liver disease and portal hypertension.
Article Title: Sex-specific differences in preclinical models of advanced chronic liver disease and portal hypertension.
Article References:
Aristu-Zabalza, P., Andrés-Rozas, M., Boyer-Díaz, Z. et al. Sex-specific differences in preclinical models of advanced chronic liver disease and portal hypertension.
Biol Sex Differ 16, 39 (2025). https://doi.org/10.1186/s13293-025-00721-8
Image Credits: AI Generated
DOI:
Keywords: Chronic liver disease, portal hypertension, sex differences, estrogen, testosterone, preclinical models, personalized medicine.